Original Article - (2021) Volume 16, Issue 3
Trans-abdominal Sonography During Intrauterine Contraceptive Device Insertion In Outpatients Setting
Ihab I. Samaha1, Ibrahim A. Abdelazim2,3* and Tamer E. El-Ghazaly2Received: 30-Aug-2021 Published: 28-Sep-2021
Abstract
Background: Pain during intrauterine contraceptive device (IUCD) insertion may be a barrier to choose the IUCD as contraceptive method. The trans-abdominal sonographic (TAS) guided IUCD insertion may decrease the IUCD insertion pain and may increase the proper positing of IUCD.
Objectives: To detect whether the use of TAS during IUCD insertion in outpatients setting is useful or not.
Methods: Three hundred (300) women eligible for IUCD insertion were included in this study and randomized into two groups (150 women in each group). TAS-guided IUCD insertion (TAS-IUCD insertion) group and non-TAS-IUCD insertion group (no ultrasound used during IUCD insertion). In the TAS-IUCD insertion group, the IUCD was applied with moderately full bladder under TAS guide without uterine sounding. While, in non-TAS-IUCD insertion group, the IUCD was applied without ultrasound guide using the routine IUCD insertion technique and uterine sounding. Participants were interviewed immediately after IUCDs insertion to report the pain intensity during IUCD insertion using visual analogue scale (VAS) and examined 4-6 weeks after IUCDs insertion by trans-vaginal sonography (TVS) to detect the intrauterine position of the inserted IUCDs. Collected data were statistically analysed to detect whether the use of TAS during IUCD insertion in outpatients setting is useful or not.
Results: There was no significant difference between TAS-IUCD insertion group and non-TAS insertion group regarding the rate of IUCD expulsion (0.7% (1/150) versus 1.3% (2/150), respectively, P=0.6), and rate of IUCD embedment (0.7% (1/150) versus 2% (3/150), respectively, P=0.3). The rate of displaced IUCDs was significantly lower in TAS-IUCD insertion group compared to non-TAS insertion group (0% (0/150) versus 2% (3/150), P=0.03). The mean pain score was significantly lower in TAS-IUCD insertion group compared to non-TAS insertion group (1.3 ± 1.02 versus 1.6 ± 0.76, P=0.0001).
Conclusion: The pain score and the rate of displaced IUCDs were significantly lower in TAS-IUCD insertion group compared to non-TAS insertion group. The use of TAS during IUCDs insertion in outpatients setting is clinically useful, it decreases the pain score during IUCDs insertion, and it decreases the rate of displaced IUCDs.
References
Blog - Find Lawyer in Oregon Best Betting Sites in Spain Best Betting Sites in Ethiopia Best Betting Sites in France Blog - Find Lawyer in New Jersey Best Betting Sites in Sweden Blog - Find Lawyer in Missouri Find Lawyer in California Blog - Find Lawyer in Georgia Find Lawyer in Louisiana Blog | Chinese Food Recipes Thai Food Recipes Blog | French Food Recipes Blog | Indian Food Recipes Casino Sites in South Africa Blog | Italian Food Recipes Best Betting Sites in India Blog | Japanese Food Recipes Find Lawyer in Florida Blog | Korean Food RecipesKeywords
Trans-abdominal sonography; Intrauterine contraceptive device; Outpatients Setting; TAS; IUCD
Abbreviations
IUCD: Intrauterine Contraceptive Device; TAS-IUCD: Trans-Abdominal Sonography Guided-Intrauterine Contraceptive Device; VAS: Visual Analogue Scale
Introduction
The intrauterine contraceptive device (IUCD) is reliable long-acting reversible method of contraception [1]. The IUCD is the first-line contraceptive method for breast-feeding women or women with history of deep venous thrombosis (DVT), thrombo-embolic disorders and/or coronary events [2].
The incidence of pregnancy with IUCD users is less than 2 per 100 woman-5 years [3]. The incidence of IUCD expulsion is 5-10% within 5 years. Uterine perforation during IUCD insertion is rare (0.6-16 cases per 1000 insertions), and the risk of perforation is high when the IUCD inserted within less than 4-6 weeks after delivery or elective abortion [2]. Pain during IUCD insertion may be a barrier to choose the IUCD as contraceptive method. The trans-abdominal sonography (TAS) guided IUCD insertion may decrease the IUCD insertion pain and may increase the proper positing of IUCD [1-4]. In addition, the TAS-guided IUCD insertion may decrease the IUCD insertion complications such as perforation, malposition, expulsion and may subsequently increases its clinical efficacy [5,6]. Therefore, this study designed to detect whether the use of TAS during IUCD insertion in outpatients setting is useful or not.
Materials and Methods
Three hundred (300) women eligible for IUCD insertion were included in this prospective study, which conducted over one year from March 2020 until March 2021, after written consent in accordance with Helsinki declaration and according to hospitals protocol.
The participants were randomly assigned using a computer-generated randomization tables into two groups (150 women in each group).
Trans-abdominal sonography-guided IUCD insertion (TAS-IUCD insertion) group and non-TAS-IUCD insertion group (no ultrasound used during IUCD insertion). (Fig. 1)
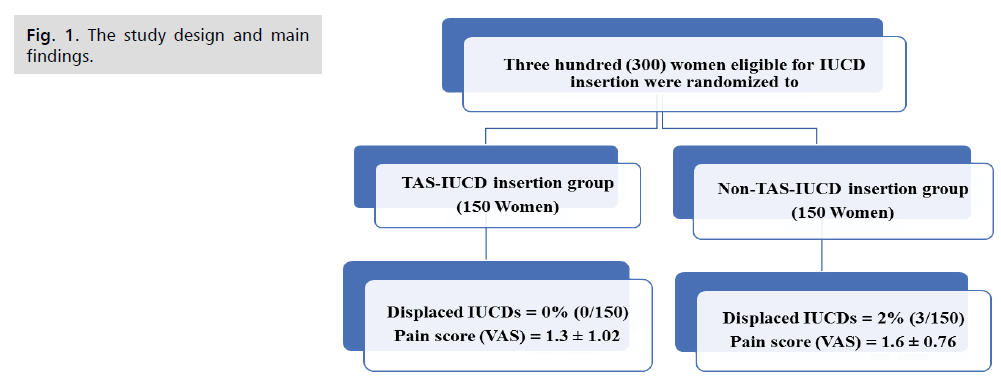
Figure 1: The study design and main findings.
Inclusion criteria include: 1) Breast-feeding. 2) Hypertensive women. 3) Women with previous history of pelvic surgery and/or endometriosis. 4) Women with history of deep venous thrombosis (DVT), or thrombo-embolic disorders. 5) Women with coronary events [7].
Exclusion criteria include: 1) Amenorrheic women (suspected pregnancy). 2) Women with gestational trophoblastic disease (persistently high β-hCG). 3) Ongoing pelvic inflammatory disease (PID). 4) Distorted uterine cavity (i.e., fibroids and/or congenital uterine anomalies). 5) Uterine length ≤6 cm or ≥10 cm. 6) Undiagnosed uterine bleeding. 7) Suspected cervical cancer or newly diagnosed endometrial cancer [7].
Contraceptive mechanism of IUCD and failure rate: The copper T380A IUCD is a T-shaped polyethylene frame wrapped with copper wire. It is FDA approved as reversible method of contraception for 10-year [7].
The exact mechanism of the copper T380A IUCD as contraception is unclear, but suggested theories include inhibition of sperm migration and viability, change in the ovum transport, and ovum damage [8].
The pregnancy rate in the first year of IUCD use is 0.6% and it is 1.9% at 10 years of IUCD use [9].
Participants counselling: Participants were counselled before IUCDs insertion regarding the available, alternative contraceptive methods.
Each participant decided to use the IUCD as contraception informed that mild pain is expected during IUCD insertion, and they signed a written consent include the possible complications of IUCD insertion.
The IUCD insertion technique: IUCDs were inserted 5-7 days post-mensural (to exclude pregnancy), without anesthesia or analgesia and after negative screening for sexually transmitted diseases (STDs) [10]. Low risk women for STDs can be screened for STDs, during IUCD insertion [11].
Participants were positioned in dorsal lithotomy position, followed by bimanual examination to confirm the uterine size and position.
Using sterile-gloves, a vaginal speculum was inserted to visualize the uterine cervix, followed by cleaning of the cervix and vagina by povidone-iodine.
A single tooth tenaculum used to grasp the anterior lip of the cervix with gentle traction to bring the cervical canal and uterine cavity in one-line in order to facilitate uterine sounding, and IUCD insertion.
The uterine sounding step was escaped in TAS-IUCD group (no uterine sounding was done in TAS-IUCD group).
The copper T380A pack was opened by an assistant and loaded inside the insertion tube by folding its two horizontal arms down along its vertical arm inside insertion tube.
The blue flange of the insertion tube was set at level equal to uterine length measured by uterine sound. The loaded insertion tube was passed through the cervical canal until the resistance of uterine fundus felt and the blue flange should be at external cervical os.
The insertion tube was withdrawn approximately 1 cm, to release the IUCD inside the uterus. The insertion tube was then gently moved up to uterine fundus to ensure placing of the IUCD at uterine fundus. While, holding the insertion tube steady, the white rod was withdrawn gentle, followed by withdrawal of the insertion tube.
Then, the IUCD strings, was visualized in the vagina, and trimmed using long scissor at approximately 3 cm length (to be easily visible outside the cervix) [7].
Participants were asked to feel the IUCD strings on regular basis at home to ensure correct IUCD placement.
In TAS-IUCD insertion group, the IUCD was inserted with moderately full bladder under TAS guide using tans-abdominal probe (Alio 400, Toshiba, Japan) without uterine sounding.
While, in non-TAS-IUCD insertion group, the IUCD was inserted without ultrasound guide using the routine IUCD insertion technique and uterine sounding.
IUCDs were inserted by MD gynecology consultant (IAA) in outpatients setting, and participants were interviewed by another consultant (TEG) blinded to methods of insertion (to avoid potential bias) immediately after IUCDs insertion, and 4-6 weeks after IUCDs insertion.
During the immediate interview, participants were asked to report the pain intensity using visual analogue scale-VAS (0 means lowest scale: no pain, while 10 means highest scale: unbearable pain).
During the 4-6 weeks interview, participants were asked about symptoms suggestive of IUCD complications (perforation, expulsion, or amenorrhea), and examined by vaginal speculum to visualize the IUCD strings and by trans-vaginal sonography (TVS) to detect the intrauterine position of IUCDs.
Uterine perforation defined as IUCD penetration through myometrium and serosa, suspected when there is severe pain or loss of resistance during uterine sounding or during IUCD insertion and absence of IUCD strings during follow-up.
IUCD embedment defined as IUCD penetration into the myometrium, but not through uterine serosa [12]. IUCD expulsion defined as passage of IUCD through the external cervical os [12], suspected when the participants fail to feel the IUCD strings, confirmed by speculum examination and TVS on follow-up.
Pregnancy should be excluded using pregnancy test or β-hCG in women complaining of amenorrhea after IUCD insertion.
Properly placed IUCD can be seen during ultrasound examination as straight hyperechoic structure in uterine cavity with its transverse arms extending laterally at uterine fundus [1,12].
Mal-positioned IUCD means abnormal rotated IUCD (longitudinal arm up and transverse arms down) [13]. Displaced IUCD means IUCD in lower uterine segment (LUS) or in cervical canal [13].
Collected data were statistically analyzed to detect whether the use of TAS during IUCD insertion in outpatients setting is useful or not.
Sample size
The required sample size for this study was calculated using G Power software version 3.1.9.7 for sample size calculation, setting α -error probability at 0.05, power (1-β error probability) at 0.95%, and effective sample size (w) at 0.5. An effective sample ≥220 women in two groups was needed to produce statistically acceptable figure.
Statistical analysis
Numerical variables were presented as mean and standard deviation (+SD), while categorical variables were presented as number and percentage. Chi-square test (X2), and Student (t) test were used for analysis of qualitative, and quantitative variables, respectively. P-value <0.5 was considered significant.
Results
There was no significant difference between TAS-IUCD insertion group and non-TAS insertion group regarding, the mean age (29.2 ± 3.4 years versus 28.4 ± 4.5, respectively), parity (4.0 ± 3.8 versus 5.1 ± 3.4, respectively), number of previous (CSs) cesarean sections (3.0 ± 2.1 versus 2.5 ± 2.4, respectively), body mass index (BMI), (31.5 ± 8.2 Kg/m2 versus 29.5 ± 7.6, respectively), and duration of IUCD insertion (4.3 ± 3.3 min. versus 3.9 ± 4.1, respectively) (Tab. 1.).
| Variables | TAS-IUCD insertion (150 Women) |
Non-TAS-IUCD insertion (150 women) |
P-value (95% Confidence Interval) |
|---|---|---|---|
| Age (years) | 29.2 ± 3.4 | 28.4 ± 4.5 | 0.9 (-0.11, 0.8, 1.71) |
| Parity | 4.0 ± 3.8 | 5.1 ± 3.4 | 0.08 (-1.9, -1.1, -0.28) |
| Number of previous CSs | 3.0 ± 2.1 | 2.5 ± 2.4 | 0.9 (-0.013, 0.5, 1.013) |
| BMI (Kg/m2) | 31.5 ± 8.2 | 29.5 ± 7.6 | 0.1 (0.005, 1.8, 3.595) |
| Duration of IUCD insertion (min.) | 4.3 ± 3.3 | 3.9 ± 4.1 | 0.9 (-0.45, 0.4, 1.25) |
| Pain score (VAS score) | 1.3 ± 1.02 | 1.6 ± 0.76 | 0.0001 × (-0.51, -0.3, -0.095) |
| IUCD Expulsion | 0.7% (1/150) | 1.3% (2/150) | 0.6 |
| IUCD embedment | 0.7% (1/150) | 2% (3/150) | 0.3 |
| Displaced IUCDs | 0% (0/150) | 2% (3/150) | 0.03* |
| Properly placed IUCDs | 98.6% (148/150) | 94.7% (142/150) | 0.8 |
Chi-square (x2) used for statistical analysis when data presented as number and percentage (%).
CSs: Cesarean Sections. Data presented as mean SD (standard deviation), number and percentage (%).
IUCD: Intrauterine Contraceptive Device.
Student t test used for statistical analysis when data presented as mean ± SD.
TAS-IUCD: Trans-Abdominal Sonographic Guided IUCD Insertion. VAS: Visual Analogue Score.
Tab. 1. Characteristic of the two-studied groups and outcome of TAS-IUCD insertion compared to non-TAS-IUCD insertion.
There was no significant difference between TAS-IUCD insertion group and non-TAS insertion group regarding the rate of IUCD expulsion (0.7% (1/150) versus 1.3% (2/150), respectively, P=0.6), and IUCD embedment (0.7% (1/150) versus 2% (3/150), respectively, P=0.3) (Tab. 1.).
The rate of displaced IUCDs was significantly lower in TAS-IUCD insertion group compared to non-TAS insertion group (0% (0/150) versus 2% (3/150), P=0.03) (Fig. 1.).
No perforations or pregnancies or mal-positioned IUCDs recorded in this study. The mean pain score was significantly lower in TAS-IUCD insertion group compared to non-TAS insertion group (1.3 ± 1.02 versus 1.6 ± 0.76, P=0.0001) (Tab. 1.).
Discussion
There was no significant difference between the two-studied groups regarding, the mean age (P=0.9), parity (P=0.08), number of previous CSs (P=0.9), BMI (P=0.1), and duration of IUCD insertion (P=0.9). Also, there was no significant difference between the two-studied groups regarding the rate of IUCD expulsion (P=0.6), and IUCD embedment (P=0.3).
Abass et al., compared the TAS-IUCD insertion to uterine sound sparing application (USSA) in which they used TVS for assessment of uterine length and position before IUCD insertion instead of uterine sounding and they recommend the use of TVS before IUCD insertion and at follow up to detect IUCD complications [1].
In this study, the IUCDs were applied under TAS guide to spare the uterine sounding step in TAS-IUCD insertion group while the routine IUCD insertion technique with uterine sounding was used in non-TAS-IUCD insertion group. Then, another TVS was done for all participants at the follow-up visit (4-6 weeks post IUCD insertion) to detect IUCD complications.
Abass et al., found the USSA was significantly shorter with high satisfaction rate [1]. Similarly in this study the TAS-IUCD insertion (without uterine sounding step) had significantly lower pain score compared to non-TAS-IUCD insertion (1.3 ± 1.02 versus 1.6 ± 0.76, respectively, P=0.0001).
Dakhly and Bassiouny, compared TAS-IUCD insertion technique by traditional IUCD insertion technique and found that TAS-IUCD insertion was statistically superior to traditional IUCD insertion technique regarding the pain scores reported by participants (P<0.001) [14].
Although, Dakhly and Bassiouny, cannot explain why the pain score was significantly less in TAS-IUCD insertion technique compared to traditional IUCD insertion technique [14].
In this study, the reduced pain during TAS-IUCD insertion can be explained by sparing the uterine sounding step in TAS-IUCD insertion technique. In addition, IUCDs insertion under ultrasound guide avoids unnecessary manipulations (touch/push) of the cervix or uterus which more likely to occur during traditional blind IUCDs insertion and causing more pain.
Maguire et al., also found the pain associated with uterine sounding could be similar or even worse than that of IUD insertion [15].
The rate of displaced IUCDs in this study was significantly lower in TAS-IUCD insertion group compared to non-TAS insertion group (0% versus 2%, respectively, P=0.03).
Moreover, Balica et al., concluded that the TAS-guided IUCD insertion allows proper IUCD placement and reduces the risk of expulsion and mal-positioning. Which may potentially decrease the risk of unintended pregnancies, post-procedural pain, and dissatisfaction with IUCD use [16].
Anteby et al., found the odds ratio for pregnancy with displaced intracervical IUCD was 13.93 (95% CI: 4.13-48.9) compared to properly placed IUCD [6].
Anteby et al., concluded that the failed contraceptive action of the IUCD may be secondary to mal-positioned device, and they recommend sonographic survey to identify displaced IUCDs [6].
McCool studied the clinical usefulness of ultrasound at IUD post insertion visit and found that 21% of symptomatic women required IUCD removal (19% due to abnormal IUCD position), and 18% of asymptomatic women required IUCD removal based on ultrasound findings [13].
McCool, support the routine use of ultrasound at IUCD post insertion visit in both symptomatic and asymptomatic women [13].
No perforations or pregnancies or mal-positioned IUCDs recorded in this study. Also, there were no perforations, or pregnancies identified in any of the eighty-four (84) asymptomatic women of McCool, study [13].
The incidence of pregnancy in IUCD users is less than 2 per 100 woman-5 years [3]. Uterine perforation during IUC D insertion is rare (0.6-16 cases per 1000 insertions), and the risk of perforation is high when IUCD inserted within less than 4-6 weeks after delivery or elective abortion [2].
This study found the pain score and the rate of displaced IUCDs were significantly lower in TAS-IUCD insertion group compared to non-TAS insertion group. This study concluded that the use of TAS during IUCDs insertion in outpatients setting is clinically useful, it decreases the pain score during IUCDs insertion, and it decreases the rate of displaced IUCDs.
This study was the first prospective randomized study conducted in Kuwait to detect whether the use of TAS during IUCD insertion in outpatients setting is useful or not.
Women refused to participate and/or give consent and the short study duration were the limitations of this study.
Future larger studies are needed to detect the long-term sequence of using IUCDs as contraceptive method (i.e., PID, ectopic pregnancies, and IUCD failure rates).
Conclusion
The pain score and the rate of displaced IUCDs were significantly lower in TAS-IUCD insertion group compared to non-TAS insertion group. The use of TAS during IUCDs insertion in outpatients setting is clinically useful, it decreases the pain score during IUCDs insertion, and it decreases the rate of displaced IUCDs.
Conflict of Interests
Authors declare no conflict of interests related to this study.
Financial Support
Nil
References
- Abbas A, Ali MK, Abdalmageed OS, et al. Evaluation of a novel uterine sound sparing approach for copper intrauterine device insertion. Fertil Steril. 2017;108(3):e123
- Intrauterine devices: an effective alternative to oral hormonal contraception. Prescrire Int. 2009;18(101):125-30.
- ESHRE Capri Workshop Group. Intrauterine devices and intrauterine systems. Hum Reprod Update. 2008;14(3):197-208.
- Committee on Practice Bulletins Gynecology, Long-Acting Reversible Contraception Work Group. Practice Bulletin No. 186: Long-Acting Reversible Contraception: Implants and Intrauterine Devices. Obstet Gynecol. 2017;130(5):e251-e269.
- Braaten KP, Benson CB, Maurer R, et al. Mispositioned intrauterine contraceptive devices: risk factors, outcomes, and future pregnancies. Obstet Gynecol. 2011;118(5):1014-20.
- Anteby E, Revel A, Ben-Chetrit A, et al. Intrauterine device failure: relation to its location within the uterine cavity. Obstet Gynecol. 1993;81(1):112-4.
- World Health Organization. Intrauterine devices (IUDs). Medical Eligibility Criteria for Contraceptive Use. 4th ed. Geneva, Switzerland: World Health Organization; 2010. 65-78.
- Rivera R, Yacobson I, Grimes D. The mechanism of action of hormonal contraceptives and intrauterine contraceptive devices. Am J Obstet Gynecol. 1999;181(5 Pt 1):1263-9.
- Trussell J. Contraceptive failure in the United States. Contraception. 2011;83(5):397-404.
- ACOG Practice Bulletin No. 121: Long-acting reversible contraception: Implants and intrauterine devices. Obstet Gynecol. 2011;118(1):184-96.
- Vidal F, Paret L, Linet T, et al. Contraception intra-utérine. RPC Contraception CNGOF [Intrauterine contraception: CNGOF Contraception Guidelines]. Gynecol Obstet Fertil Senol. 2018;46(12):806-822.
- Bhute A, Bhute S. Embedded Intrauterine Contraceptive Device with Cervical Fibroid. Int J Recent Surg Med Sci. 2016; 02(01): 47-48.
- McCool R. Clinical usefulness of the IUD post insertion ultrasound in symptomatic and asymptomatic patients. Proc Obstet Gynecol. 2019; 9(2):5.
- Dakhly DMR, Bassiouny YA. Ultrasound-guided intrauterine device insertion: a step closer to painless insertion: a randomized control trial. Eur J Contracept Reprod Health Care. 2017; 22(5):349-53.
- Maguire K, Davis A, Rosario Tejeda L, et al. Intracervical lidocaine gel for intrauterine device insertion: a randomized controlled trial. Contraception. 2012; 86(3):214-9.
- Balica AC, Kim C-S, Egan S, et al. Sonographically guided insertion of intrauterine device: Indications and results. J Clin Ultrasound. 2017; 00:000-000.
Author Info
Ihab I. Samaha1, Ibrahim A. Abdelazim2,3* and Tamer E. El-Ghazaly22Department of Obstetrics and Gynecology, Faculty of Medicine, Ain Shams University, Cairo, Egypt
3Department of Obstetrics and Gynecology, Kuwait Oil Company (KOC), Ahmadi, Kuwait
Copyright:This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.