Research - (2022) Volume 17, Issue 3
Predictors of severe labour pain: prospective observational study
Anastasiia Romanenko* and Iurii KuchynReceived: 07-Sep-2022, Manuscript No. gpmp-22-73945; Editor assigned: 08-Sep-2022, Pre QC No. P-73945; Reviewed: 13-Sep-2022, QC No. Q-73945; Revised: 19-Sep-2022, Manuscript No. R-73945; Published: 30-Sep-2022
Abstract
Introduction: Pain during childbirth is a subjective experience that every mother experiences differently. The degree of a woman's suffering in childbirth depends on the intensity of labour pain and many indirect factors. Complex interrelated effects on labour pain are limited by the small number of studies available. That is why it is necessary to determine the probable factors that may affect the intensity of pain. In accordance with this, determining predictors of the intensity of women’s pain during vaginal delivery remains an important issue for maternity health policy.
Aim: Investigate predictors of severe labour pain.
Method: A prospective observational study was conducted in the period from December 2020 to May 2021 at the Kyiv City Maternity Hospital №5 (Kyiv, Ukraine). Univariate and multivariate logistic regression were used to measure the influence of risk factors on the probability of severe labour pain.
Results: The examined predictors were derived from mothers` self-report of overall childbirth. 366 women took part in research, 282 of them rated their pain by ≤ 70 mm visual analog scale (VAS), while 84 patients reported their pain by ≥ 60 mm VAS. The study identified predictors that reduce the risk of severe labour pain, such as a second delivery (OR 0.60 [95% CI 0.37–0.98], p=0,04), a woman's prenatal health (namely, a healthy prenatal woman) (OR 0.16 [95% CI 0.07–0.37], p<0.001), attendance of antenatal classes (OR 0.09 [95% CI 0.05–0.17)], p<0.001), the constant doula`s help (OR 0, 21 [95% CІ 0.12 – 0.36], p<0.001) and feeling of control over pain in labour (OR 0,05 [95% CІ 0.03–0.09], p<<0.001). In addition, predictors such as and presence of general anxiety disorder in contrast to the factors listed above, increase the risk of severe labour pain (OR 5.63 [95% CI 3.33–9.51], p<0.001).
Conclusion: These studies scientifically substantiate the importance of prenatal screening of the mental state of pregnant women and antenatal education. Our Ukrainian research suggests women, medical team and doulas should be involved in care in labour and in shared decision making for improving health outcomes.
Keywords
Severe labour pain; Doula’s support; Antenatal education
Introduction
Labour is a critical moment for every woman and her child, so any complication can significantly increase the risk of morbidity and mortality as well as overall mother satisfaction [1-3]. The WHO identifies pain as an integral part of vaginal delivery, which affects the general condition of the mother and fetus [4]. It is known that almost 80% of women, who gave birth for the first time, rate pain as "severe" or "very strong", which they will remember for a long time [5].
Every mother has the right to adequate pain relief, despite the fact that childbirth is a natural process [6]. Therefore, the main principle of modern obstetrics is to alleviate suffering from labour pain for those who wish to receive analgesia and have no medical contraindications [7-11].
Currently, most women need individual methods of analgesia [12]. There is a tendency to use neuraxial analgesia during vaginal delivery, approximately in 70% of the cases [13], which has shown higher effectiveness in pain control than systemic analgesics or inhalation methods [14].
In order to avoid the negative effects associated with the use of pharmacological methods of analgesia, some groups of women have recently focused more and more on planning childbirth with the primary use of alternative methods of analgesia [15]. For example, antenatal training helps women prepare for childbirth in order to control pain during childbirth, as well as reduce anxiety, fear, or negative expectations of childbirth [16]. However, these alternative methods have a low level of evidence regarding the reduction of pain and are individual in nature [17-22].
Due to the variety of pharmacological and non-pharmacological methods of analgesia in women, labour pain is considered debatable and, at times, divergent in its understanding by medical staff and the mother herself [23].
All of the above necessitated the study of probable factors influencing the intensity of pain in women during childbirth. As we already know, the intensity of labour pain is associated with physiological (cervical dilation and uterine contractions) [24], psychological (fear/anxiety) [25], emotional and social (partner childbirth) and demographic factors (age, level of education) [26], as well as with the previous experience of childbirth, certain features of the country's culture and ethnicity of women [27]. Doula’s support is not very popular in Ukraine.
In Ukraine, there are still few studies on possible predictors of severe labour pain. The primary study hypothesis was that attendance of antenatal classes, constant doula’s assistance, and feeling in control of pain reduced the risk of severe labour pain. A secondary hypothesis is that the presence of generalized anxiety disorder increases the risk of severe labour pain. This study is needed to improve shared decision-making at different levels in maternity care.
Aim
Investigate predictors of severe labour pain.
Materials and Methods
A prospective observational study was conducted in the period from December 2020 to May 2021 at the Kyiv City Maternity Hospital No.5.
Inclusion criteria: Mothers over 18years of age, uncomplicated pregnancy, intended vaginal delivery and Caesarean delivery at 37-41 gestation age; 1st or 2nd parturitions; childbirth with the birth of the singleton live fetus.
Exclusion criteria: Mothers over 45 years of age; inability to obtain the informed consent of the patient or their legal representative; persistent opioid users.
The study protocol №170 was approved by the Bogomolets National Medical University Ethics Committee.
During vaginal delivery, patients reported their pain level using a visual analogue scale (VAS). The intensity of pain was determined depending on the position of the mother in which she gave birth; during/between contractions; at rest.
The main objective of the study is measurement of severe labour pain, which is the subjective feeling of patients with a determined pain level ≥ 70 mm using a visual analogue scale (VAS).
Depending on the intensity of pain, women in labour were divided into 2 groups:
Group 1 (n=282) - women with severe labour pain by level by VAS ≥ 70 mm
Group 2 (n=84) - women with no severe labour pain level by VAS ≤ 60 mm
In the postpartum period all patients filled in questionnaires and underwent interviews from the 1st to the 3rd day after delivery. The following groups of risk factors were studied:
1) Demographic indicators (age, level of working capacity 2 months before childbirth). Work capacity is evaluated according to the following parameters: "0" - no, "1" - yes.
2) General level of health (woman's level of health before childbirth, daily physical activity before childbirth, bad habits - smoking during pregnancy). Regarding the assessment of the level of the woman's prenatal health, in our questionnaire, we used the following indicators: "0" – poor, "1" – good. Regarding daily physical activity during pregnancy, this indicator is estimated from 1 to 4 points (0 - (less than 30 minutes per day), 1 - (30 minutes - 1 hour per day), 2 - (1-2 hours per day), 3 - (2-3 hours a day), 4 - (more than 3 hours a day).
3) Presence of mental disorders before childbirth (level of anxiety 2 weeks before childbirth, widespread muscle pain with fatigue or problems with memory, sleep, and mood). The prenatal level of anxiety was assessed using the general anxiety disorder scale-2 (GAD-2), where ≤ 3 points is considered a positive result of detecting such a disorder.
4) Prenatal preparation (attendance at maternity school, feeling of control over pain in labour). Education at the maternity school was evaluated as: "0" - no, "1" - yes. A woman's ability to control pain was assessed: "0" - no, "1" - yes.
5) The level of assistance during childbirth (constant support from a doula during childbirth, the woman's ability to control pain in childbirth). The constant help of a doula was evaluated on the following scale, where "0" - (no doula help) and "1" to "4" points - (quality of doula help). The woman's ability to control pain in childbirth was evaluated as: "0" - no, "1" - yes.
Statistical analysis of the research results was carried out using the EZR v package. 1.54 [19]. Differences between the mean values of indicators were evaluated using the Student's t-test, after confirming the normal distribution of the data using the Shapiro-Wilk test. The method of building logistic regression models was used to identify factors that affect the intensity of labour pain. The predictive qualities of logistic regression models were evaluated by the area under the operating characteristics curve (ROC curve) of the model - Area under the ROC curve (AUC), its 95% confidence interval (95% CI) was calculated. To assess the degree of influence of factor characteristics on the resulting variable, the odds ratio (OR) and its 95% CI were calculated. The sensitivity and specificity of the model were calculated. In all statistical tests, the statistical significance was p = 0.05.
Results
The study involved 366 patients. Group 1 included 282 patients (pain level ≥70 mm according to the VAS). Group 2 included 84 patients (pain level ≤ 60 mm using the VAS). In both groups there was no significant difference in age: in group 1 - (29.7 ± 5.1), and in group 2 - (29.3 ± 4.7) (p = 0.4963).
The method of building logistic regression models was used in the analysis of the relationship between the risk of severe labour pain (women with VAS scores ≥70 mm) and factor variables. The analysis was performed for ten risk factors. Tab. 1. presents the results of the univariate analysis.
| Factor variables | Coefficient b ± m |
p | OR (95% CІ) | |
|---|---|---|---|---|
| Age | –0.064 ± 0.025 | 0.011 | 0.93 (0.89 – 0.98) |
|
| Parturitions | First | - | ||
| Second | –0.52 ± 0.25 | 0.040 | 0.60 (0.37 – 0.98) |
|
| Attendance of antenatal classes | No | - | ||
| Yes | –2.39 ± 0.31 | <0.001 | 0.09 (0.05 – 0.17) |
|
| Woman's prenatal health | Not very healthy | - | ||
| Healthy | –1.86 ± 0.44 | <0.001 | 0.16 (0.07 – 0.37) |
|
| General anxiety disorder | No | - | ||
| Yes | 1.72 ± 0.27 | <0.001 | 5.63 (3.33 – 9.51) |
|
| Constant support from the doula | No | - | ||
| Yes | –1.56 ± 0.27 | <0.001 | 0.21 (0.12 – 0.36) |
|
| Daily physical activity before childbirth | –0.10 ± 0.10 | 0.283 | – | |
| Feeling of control over pain in labour | No | - | ||
| Yes | –3.00 ± 0.31 | <0.001 | 0.05 (0.03 – 0.09) |
|
| Work during the last two months before childbirth | No | - | ||
| Yes | –0.15 ± 0.28 | 0.579 | – | |
| Smoking during pregnancy | No | - | ||
| Yes | –0.54 ± 0.56 | 0.334 | – | |
Tab. 1. Coefficients of univariate logistic regression models for predicting the risk of severe labour pain.
To identify a group of signs associated with the risk of severe labour pain, indicators were selected using the method of stepwise inclusion/exclusion of factor signs (Stepwise, with an inclusion threshold of p<0.05 and an exclusion threshold of p>0.1). Out of ten risk factors, 4 independent characteristics were identified: attendance of antenatal classes, woman's prenatal health, presence of general anxiety disorder, and feeling of control over pain in labour. Fig. 1. shows the operating characteristic curve of the four-factor model.
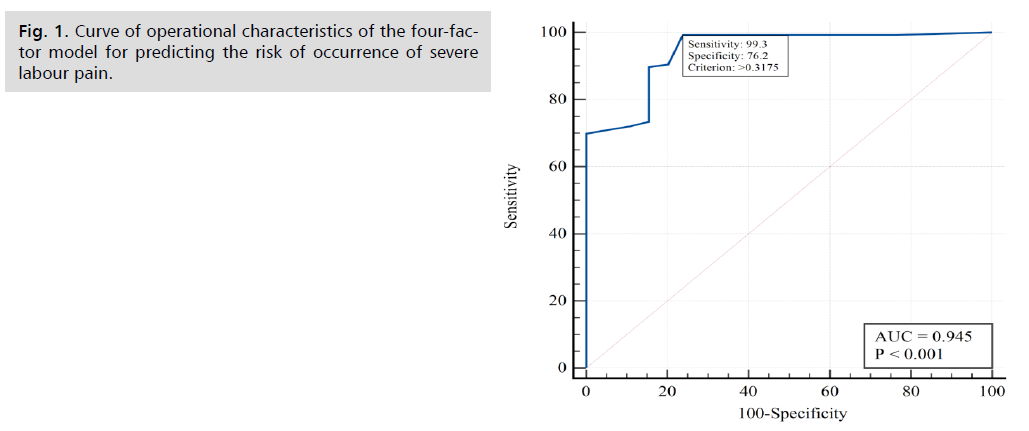
Fig 1. Curve of operational characteristics of the four-factor model for predicting the risk of occurrence of severe labour pain.
The analysis revealed (see Tab. 1.) a decrease (p=0.040) in the risk of severe labour pain for second births in the early stages (72.3% of cases), OR = 0.60 (95% CI 0.37–0.98) compared to first births (81.3% cases of severe labour pain).
According to our study, which showed a reduction (p<0.001) in the risk of severe labour pain when attending antenatal classes (53.7% of cases), (AUC = 0.77 95% CI 0.72 – 0.81) compared to the group that did not attend antenatal classes (92.7% of cases of severe labour pain).
With a healthy prenatal woman, the risk of developing severe labour pain (70.8% of cases) decreases (p<0.001), (OR = 0.16 (95% CI 0.07–0.37) in comparison with the group of women with poor prenatal health (93.9% of cases severe labour pain).
In the course of the study, it was found that in the presence of general anxiety disorder, the risk of developing severe labour pain (86.4% of cases) increases (p<0.001), OR = 5.63 (95% CI 3.33–9.51) in comparison with the group of women without this disorder (86.4% of cases of severe labour pain).
A reduction (<0.001) in the risk of severe labour pain (61.8% of cases) was also found for women who used constant doula`s help, (OR = 0.21 (95% CI 0.12 – 0.36) compared to the group that did without a doula`s help (88.5% of severe labour pain cases).
In our study, for women with a feeling of control over pain in labour, the risk of severe labour pain (35.1% of cases) is reduced, (OR = 0.05 (95% CI 0.03–0.09), AUC = 0.81 (95%CI 0.76–0.84)) compared to those who did have a feeling of control (91.5% of cases of severe labour pain). In the research groups there were no significant differences in such factors as daily physical activity during pregnancy (p = 0.283); work during the last two months before childbirth (p = 0.579); smoking during pregnancy (p = 0.334);
Discussion
Women are no longer satisfied with inadequate pain relief during vaginal delivery, which negatively affects their mental state, increasing the risk of postpartum depression/post-traumatic stress disorder following childbirth, increasing the number of future abortions, caesarean sections, negative emotions towards the newborn, and breastfeeding problems [28]. This is why a woman's mental state, including the pre-threshold level of anxiety, not only affects a woman's satisfaction with labour and childbirth but also the intensity of pain. In this study, a prenatal assessment of general anxiety disorder was conducted and the results showed that those mothers whose score was greater than or equal to 3 - had an increased risk of severe labour pain in relation to parturients for whom the assessment of the severity of pain is less than 3 points (p<0.001). Our data are consistent with the results of a foreign study on anxiety associated with labour pain and labour outcomes [29]. Our study showed that the second birth decreases the risk of severe labour pain compared with women who have first childbirths before (p=0.04). It was proved that women who attended antenatal classes had a higher level of confidence in their ability to cope with labour pain and manage the birth process, compared with those who did not attend it (p = 0.05) [30-31], which is fully compatible with the data from our study, which showed that in patients who did not attend antenatal classes, the risk of severe labour pain increased compared to those patients who attended it (p <0,001). Patients who rated their prenatal health status as " not very healthy " had an increased risk of severe labour pain compared with patients who rated their health status as "healthy" prior to delivery (p <0,001).
Also, there was no association between daily physical activity and the risk of severe labour pain (p = 0.80057) [32-34]. But to confirm or refute the hypothesis of a positive effect of physical activity on childbirth, we need separate tests, with properly designed exercise programs. At this stage, our study did not reveal the effect of this factor on the reduction of pain in women during vaginal delivery (p = 0.283).
Regarding doula care during childbirth: the risk of severe pain decreased in the group of women who used the help of a doula. The study showed that patients who used the constant support from doula reduced the risk of severe pain in relation to patients who did not use the help of a doula (p <0.001). Cochrane meta-analyses involving 12,433 women found no evidence of a negative impact of the continued support during childbirth and believe that doula care during childbirth reduces the risk of using any type of analgesia (such as epidural analgesia) [ 35-36]. If we talk about the factor of feeling pain control during childbirth, we should note the statistics of the Dutch study, in which the majority of women, 25.7% (out of 104), had poor control of pain during childbirth [37]. These data are fully consistent with the results of our study, which showed that patients who had less pain control during childbirth had an increased risk of severe labour pain compared with patients who controlled pain well (OR 0.1266 [95% CI 0, 0711 - 0.2255], p<0.001). The extent to which a woman experiences pain control is an important indicator of a mother's self-efficacy and emotional well-being during childbirth [38-40]. A woman's feeling of pain control is considered an important indicator of a woman's subsequent psycho-emotional well-being, which, in the absence of it, causes a negative or even traumatic experience of childbirth [29].
Conclusion
These studies scientifically substantiate the importance of prenatal screening of the mental state of pregnant women and antenatal education. Our Ukrainian research suggests women, medical team and doulas should be involved in care in labour and in shared decision making for improving health outcomes.
References
- Karlsdottir SI, Sveinsdottir H, Kristjansdottir H, et al. Predictors of women’s positive childbirth pain experience: findings from an Icelandic national study. Women Birth. 2018;31(3):e178-e184.
- Madden KL, Turnbull D, Cyna AM, et al. Pain relief for childbirth: The preferences of pregnant women, midwives and obstetricians. Women Birth. 2013;26(1):33-40.
- Lowe NK. The nature of labor pain. Am J Obstet Gynecol. 2002;186(5):S16-S24.
- World Health Organization. The prevention and elimination of disrespect and abuse during facility-based childbirth: WHO statement. WHO. 2014.
- Waldenström U, Schytt E. A longitudinal study of women’s memory of labour pain—from 2 months to 5 years after the birth. BJOG: Int J Obstet Gynaecol. 2009;116(4):577-583.
- Fang X, Huan Y, Tao Y, et al. Incidence, severity, and determinants of uterine contraction pain after vaginal delivery: a prospective observational study. Int J Obstet Anesth. 2021 May 1;46:102961.
- American College of Obstetricians and Gynecologists. ACOG practice bulletin no. 209: obstetric analgesia and anesthesia. Obstet Gynecol. 2019;133(3):e208-e225.
- Carlier L, Devroe S, Budts W, et al. Cardiac interventions in pregnancy and peripartum–a narrative review of the literature. J Cardiothorac Vasc Anesth. 2020;34(12):3409-3419.
- Arendt KW, Lindley KJ. Obstetric anesthesia management of the patient with cardiac disease. Int J Obstet Anesth. 2019;37:73-85.
- Benjamin EJ, Virani SS, Callaway CW, et al. Heart disease and stroke statistics—2018 update: a report from the American Heart Association. Circulation. 2018;137(12):e467-492.
- Knight M, Bunch K, Tuffnell D, et al. Saving Lives, Improving Mothers’ Care-Lessons learned to inform maternity care from the UK and Ireland Confidential Enquiries into Maternal Deaths and Morbidity 2014-16. National Perinatal Epidemiology Unit: University of Oxford; 2018.
- Anim‐Somuah M, Smyth RM, Cyna AM, et al. Epidural versus non‐epidural or no analgesia for pain management in labour. Cochrane Database Syst Rev. 2018(5).
- Hemant K Satpathy. Labor and Delivery, Analgesia, Regional and Local. Medscape. 2020; 29.
- Chau A, Bibbo C, Huang CC, et al. Dural puncture epidural technique improves labor analgesia quality with fewer side effects compared with epidural and combined spinal epidural techniques: a randomized clinical trial. Anesth Analg. 2017;124(2):560-569.
- Caughey AB, Tilden E. Nonpharmacologic approaches to management of labour pain. UpToDate. Waltham, MA: UpToDate. 2004.
- Cutajar L, Miu M, Fleet JA, et al. Antenatal education for childbirth: Labour and birth. Eur J Midwifery. 2020;4.
- Cluett ER, Burns E, Cuthbert A. Immersion in water during labour and birth. Cochrane Database Syst Rev. 2018(5).
- Berta M, Lindgren H, Christensson K, et al. Effect of maternal birth positions on duration of second stage of labor: systematic review and meta-analysis. BMC Pregnancy Childbirth. 2019;19(1):1-8.
- Smith CA, Collins CT, Levett KM, et al. Acupuncture or acupressure for pain management during labour. Cochrane Database Syst Rev. 2020(2).
- Smith CA, Levett KM, Collins CT, et al. Massage, reflexology and other manual methods for pain management in labour. Cochrane Database Syst Rev. 2018(3).
- Boaviagem A, Junior EM, Lubambo L, et al. The effectiveness of breathing patterns to control maternal anxiety during the first period of labor: A randomized controlled clinical trial. Complement Ther Clin Pract. 2017;26:30-35.
- Junge C, von Soest T, Weidner K, et al. Labor pain in women with and without severe fear of childbirth: a population‐based, longitudinal study. Birth. 2018;45(4):469-477.
- Kacperczyk-Bartnik J, Bartnik P, Symonides A, et al. Association between antenatal classes attendance and perceived fear and pain during labour. Taiwan J Obstet Gynecol. 2019;58(4):492-496.
- Hulsbosch LP, Nyklíček I, Potharst ES, et al. Development of the Labor Pain Relief Attitude Questionnaire for pregnant women (LPRAQ-p). BMC Pregnancy Childbirth. 2020;20(1):1-2.
- Labor S, Maguire S. The pain of labour. Rev Pain. 2008;2(2):15-19.
- Lindert J, von Ehrenstein OS, Priebe S, et al. Depression and anxiety in labor migrants and refugees–a systematic review and meta-analysis. Soc Sci Med. 2009;69(2):246-257.
- World Health Organization. WHO recommendations on intrapartum care for a positive childbirth experience. WHO; 2018.
- Ye HJ, Jiang YJ, Ruan ZF. Relationship between factors of labour pain and delivery outcomes. Zhonghua fu chan ke za zhi. 2011;46(10):753-757.
- Guszkowska M. The effect of exercise and childbirth classes on fear of childbirth and locus of labor pain control. Anxiety Stress Coping. 2014;27(2):176-189.
- Barimani M, Frykedal KF, Rosander M, et al. Childbirth and parenting preparation in antenatal classes. Midwifery. 2018;57:1-7.
- Szumilewicz A, Wojtyla A, Zarebska A, et al. Influence of prenatal physical activity on the course of labour and delivery according to the new Polish standard for perinatal care. Ann Agric Environ Med. 2013;20(2).
- Marín-Jiménez N, Acosta-Manzano P, Borges‐Cosic M, et al. Association of self‐reported physical fitness with pain during pregnancy: The GESTAFIT Project. Scand J Med Sci Sports. 2019;29(7):1022-1030.
- Beebe KR, Lee KA. Sleep disturbance in late pregnancy and early labor. J Perinat Neonatal Nurs. 2007;21(2):103-108.
- Bohren MA, Hofmeyr GJ, Sakala C, et al. Continuous support for women during childbirth. Cochrane Database Syst Rev. 2017(7).
- Hollander MH, van Hastenberg E, van Dillen J, et al. Preventing traumatic childbirth experiences: 2192 women’s perceptions and views. Arch Womens Ment Health. 2017;20(4):515-523.
- Siyoum M, Mekonnen S. Labor pain control and associated factors among women who gave birth at Leku primary hospital, southern Ethiopia. BMC Res Notes. 2019;12(1):1-5.
- World Health Organization. WHO recommendations on intrapartum care for a positive childbirth experience. WHO; 2018.
- Carlsson M, Ziegert K, Nissen E. The relationship between childbirth self-efficacy and aspects of well-being, birth interventions and birth outcomes. Midwifery. 2015;31(10):1000-1007.
- Brixval CS, Axelsen SF, Thygesen LC, et al. Antenatal education in small classes may increase childbirth self-efficacy: results from a Danish randomised trial. Sex Reprod Healthc. 2016;10:32-34.
- Ray-Griffith SL, Wendel MP, Stowe ZN, et al. Chronic pain during pregnancy: a review of the literature. Int J Womens Health. 2018;10:153.
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Author Info
Anastasiia Romanenko* and Iurii KuchynCopyright:This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.