Research Article - (2023) Volume 0, Issue 0
Predictive value of complete blood count parameters in placenta accreta spectrum: A prospective cohort study
Ahmed Sherif Abd El Hamid*, Abd El Megeed Ismail Abd El Megeed, Rawhia Elsayed Mohammed Elsayed and Ahmed Mahmoud HusseinReceived: 02-May-2023, Manuscript No. gpmp-23-122485; Editor assigned: 04-May-2023, Pre QC No. P-122485; Reviewed: 18-May-2023, QC No. Q-122485; Revised: 23-May-2023, Manuscript No. R-122485; Published: 01-Jun-2023
Abstract
Background: During pregnancy, the CBC (Complete Blood Count) can be used to predict placental invasion anomalies. Studies have suggested that cancer cell invasion shares some similarities with trophoblast invasion.
Objective: To determine the prognostic role of CBC parameters for the Placenta Accreta Spectrum (PAS).
Patients and methods: We performed a prospective observational cohort study at Ain Shams University Maternity Hospital from January 2019 to December 2019 on 160 pregnant patients diagnosed with the placenta accreta spectrum. In all cases, parameters of complete blood count, including lymphocyte, platelet count, Red cell Distribution Width (RDW), neutrophil/lymphocyte ratio, and Mean Platelet Volume (MPV), were analyzed.
Results: Among the patients studied, two subgroups were analyzed: placenta previa and placenta accreta. The results show a statistically significantly lower mean value of RDW and platelets in accreta than no accreta, with a p-value (<0.05), while a statistically significantly higher mean value of MPV and N/L ratio in accreta than no accreta, with p-value (<0.05). Receiver Operator Characteristics (ROC) curves showed that RDW%, Platelets, MPV, and N/L ratio indices were significant predictors as denoted by the significantly large area under the curves (AUC;0.668, 0.635, 0.780, and 0.696) and p-value (p<0.05) with MPV being the most significant predictor.
Conclusion: CBC parameters are inexpensive, routinely feasible, and reproducible markers to help predict the Placenta accreta spectrum
Keywords
Mean platelet volume; Neutrophil/Lymphocyte (N/L); Placenta red cell distribution; Placenta previa; Placenta accreta
Introduction
Placenta accreta is defined as abnormal trophoblastic invasion of the placenta into the myometrium of the uterus in pregnancy. The Placenta Accreta Spectrum (PAS) replaces the term Morbidly Adherent Placenta (MAP). PAS includes placenta accreta if invading the decidual surface of the myometrium, placenta increta (invading more deeply within the myometrium), and placenta percreta (penetrating the uterine serosa and invading the surrounding organs such as the bladder) [1].
Placenta Accreta Spectrum (PAS) has high morbidity and 7.0% mortality rates. The maternal morbidities include obstetric hemorrhage (antepartum, intrapartum, and postpartum) requiring massive blood transfusion. There are also surgical complications, such as bladder and ureteric injuries, with most cases ending with an obstetric hysterectomy. Ultrasonography and Magnetic Resonance Imaging (MRI) are commonly used to screen and diagnose PAS, but they have their pitfalls [1,2].
Several studies have suggested that the invasion of trophoblast cells shares similarities with cancer cell invasion. Recently, the predictive value of specific inflammatory markers, such as neutrophil/lymphocyte and platelet/lymphocyte ratios obtained from pre-surgery blood counts of patients, has been assessed in ovarian and endometrial cancers [3,4].
Among other studies, this study utilizes CBC parameters that could be used with ultrasound imaging to screen for PAS disorders prenatally, aiding early referral to higher centers [5,6].
Aim of the Work
This study examines the relationship between CBC parameters and the Placenta Accreta Spectrum.
Patients and Methods
We performed a prospective observational cohort study in Ain Shams University Maternity Hospital from January 2019 to December 2019 with the diagnosis of the placenta Accreta spectrum. The study protocol gained the ethical committee approval of the Obstetrics and Gynecology Department of Ain Shams University.
Our study involved 160 women who had a previous cesarean section and were diagnosed with complete placenta previa and suspected placental accreta spectrum. To be eligible for the study, women had to be over 18 years old, have a gestational age of more than 28 weeks, and have a history of previous cesarean section. The placenta previa/accreta was diagnosed using ultrasonography, Doppler, and occasionally MRI. Women with ruptured membranes, chorioamnionitis, multiple pregnancies, or any medical disorder were excluded from the study. We also excluded women with infections or medical disorders that could affect their complete blood picture parameters [5].
Upon admission, the location of the placental implantation and the depth of myometrial invasion were identified using a Sonoace Samsung ultrasound R5 machine (2-8 MHZ, made in Korea) with transabdominal and transvaginal 2D gray scale and Doppler sonography. The ultrasonographic criteria for diagnosing the placenta accreta spectrum involves the loss of the retroplacental echo-lucent area and/or irregularity in the uteroplacental junction and myometrial thinning of less than 1 mm. Criteria suggesting bladder invasion include increased vascularity of the vesicouterine space and abnormal high-velocity blood flow in placental lacunae [5]. The diagnosis of the Placenta accreta spectrum was confirmed by histopathological examination.
The intraoperative diagnosis of the placenta accreta spectrum was confirmed at the time of cesarean section and in histopathological evaluation, whether the patient underwent a hysterectomy by the attending consultant obstetricians.
Before delivery, blood samples were obtained through venipuncture from the antecubital area of the arm, which is the most common way to collect blood from an adult patient. The samples were analyzed to predict cases with real placental invasion anomaly, with parameters such as lymphocyte count, platelet count, Red cell Distribution Width (RDW), neutrophil/lymphocyte ratio, and Mean Platelet Volume (MPV) taken into account. The blood was drawn into vacuum tubes that contained edetatetripotassium. Complete blood count parameters, including total leukocytes and platelets, were analyzed using an automated cell counter called Hemalog.
Sample Size Justification: Using the PASS program, we have set the alpha error at 5% and the confidence interval width at 0.15. The result from a previous study [6] showed that the prevalence of placenta accreta among placenta previa cases was 31.5%. With a 10% dropout rate, we decided on a sample size of 160 cases.
Statistical analysis: Recorded data were analyzed using the statistical package for social sciences, version 23.0 (SPSS Inc., Chicago, Illinois, USA). The quantitative data were presented as mean± standard deviation and ranges. Also, qualitative variables were presented as numbers and percentages. The Independent-sample t-test of significance was used when comparing two means. Receiver Operating Characteristic (ROC curve) analysis was used to determine the overall predictivity of the parameter and the best cut-off value with the detection of sensitivity and specificity at this cut-off value. The confidence interval was 95%, and the margin of error accepted was set to 5%. So, the p-value was considered significant as follows P-value <0.05 was considered significant, P-value <0.001 was considered highly significant, and P-value >0.05 was considered insignificant.
Results
Tab. 1. shows the demographic and laboratory data distribution among the study cases. There was no significant difference between the placenta previa and the accreta groups regarding the demographic data (P<0.05).
| Parameters | Mean ± SD | Range |
|---|---|---|
| Age (years) | 28.7 ± 4.0 | 22.0-37.0 |
| BMI (kg/m2) | 26.4 ± 1.7 | 21.7-31.2 |
| GA (weeks) | 37.4 ± 0.6 | 37.0-39.0 |
| RDW (%) | 16.5 ± 1.8 | 11.3-21.8 |
| Platelets (x103/mL) | 244.4 ± 57.9 | 99.3-384.2 |
| MPV (fL) | 7.9 ± 0.9 | 6.0-10.2 |
| Lymphocyte (x103/mL) | 2.4 ± 0.5 | 1.1-3.4 |
| Neutrophils (x103/mL) | 11.0 ± 3.6 | 4.0-23.5 |
| N/L ratio | 4.6 ± 1.2 | 1.5-7.6 |
| P/L ratio | 105.4 ± 33.8 | 36.8-211.1 |
Tab. 1. Demographic and laboratory data distribution among the 160 cases.
The Intraoperative and histopathological diagnosis of placenta accreta is shown in Tab. 2. and Fig. 1. Placenta accreta was confirmed in 61 patients (38.1%), and 99 (61.9%) had no accreta.
| Placenta accreta | N | % | |
|---|---|---|---|
| Intraoperative diagnosis (Total=160) |
Accreta | 76 | 47.5 |
| No accreta | 84 | 52.5 | |
| Intervention (Total=76) |
Conservative | 48 | 63.2 |
| Hysterectomy | 28 | 36.8 | |
| Conservative Biopsy (Total=48) |
Accreta | 37 | 77.1 |
| No accreta | 11 | 22.9 | |
| Hysterectomy Biopsy (Total=28) |
Accreta | 24 | 85.7 |
| No accreta | 4 | 14.3 | |
Tab. 2. Intraoperative and histopathology diagnoses among the 160 studied cases.
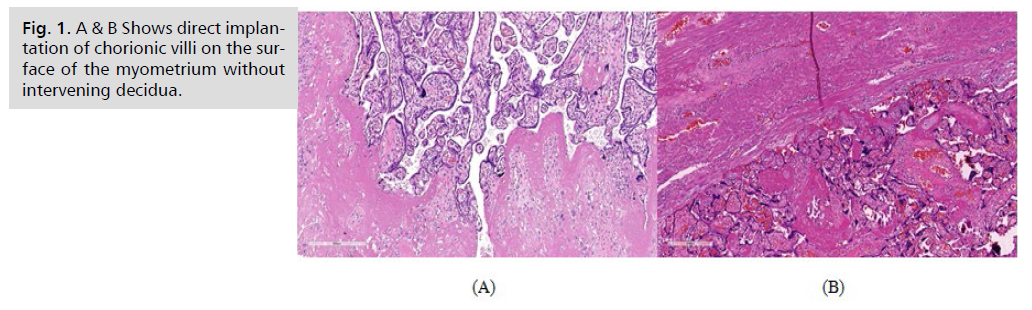
Fig 1. A & B Shows direct implantation of chorionic villi on the surface of the myometrium without intervening decidua.
Our results show a statistically significantly lower mean value of RDW and platelets in accreta than no accreta, with a p-value<0.05, while a statistically significantly higher mean value of MPV and N/L ratio in accreta than no accreta, with p-value (<0.05) (Tab. 3.).
| Variables | Accreta (N=61) |
No accreta (N=99) |
P value |
|---|---|---|---|
| RDW (%) | 15.8 ± 1.7 | 17.0 ± 1.8 | <0.001* |
| Platelets (x103/mL) | 228.8 ± 47.1 | 254.0 ± 61.9 | 0.004* |
| MPV (fL) | 8.5 ± 0.8 | 7.5 ± 0.8 | <0.001* |
| Lymphocyte(x103/mL) | 2.4 ± 0.5 | 2.5 ± 0.5 | 0.355 |
| Neutrophils(x103/mL) | 11.5 ± 0.5 | 10.6 ± 0.4 | 0.113 |
| N/L ratio | 5.1 ± 1.2 | 4.3 ± 1.1 | <0.001* |
| P/L ratio | 101.0 ± 4.0 | 108.0 ± 3.5 | 0.206 |
Tab. 3. Comparison between the accreta group and no accreta according to laboratory data.
Receiver operating characteristics were used to define the best cut-off value of different parameters (RDW%, Platelets, MPV, and N/L ratio) studied to calculate sensitivity, specificity, and negative predictive value; it showed that MPV ≥ 8.1 (fl) had the highest diagnostic characteristics in diagnosing placenta accreta. MPV ≥ 8.1 (fl) had moderate diagnostic characteristics in diagnosing placenta accreta (Tab. 4.).
| Characteristics | Value | 95% CI | Value | 95% CI | |
|---|---|---|---|---|---|
| RDW ≤ 16.6 (%) | Platelets ≤ 264.0 (x103/mL) | ||||
| Sensitivity | 77.0% | 64.5%-86.8% | 77.0% | 64.5%-86.8% | |
| Specificity | 54.5% | 44.2%-64.6% | 50.5% | 40.3%-60.7% | |
| DA | 63.1% | 55.1%-70.6% | 60.6% | 52.6%-68.2% | |
| Youden's index | 31.6% | 17.2%-46.0% | 27.6% | 13.1%-42.0% | |
| PPV | 51.1% | 40.4%-61.7% | 49.0% | 38.6%-59.4% | |
| NPV | 79.4% | 67.9%-88.3% | 78.1% | 66.0%-87.5% | |
| LR+ | 1.70 | 1.31-2.19 | 1.56 | 1.22-1.98 | |
| LR- | 0.42 | 0.26-0.69 | 0.45 | 0.28-0.75 | |
| LR | 4.03 | 1.97-8.24 | 3.43 | 1.68-7.00 | |
| MPV ≥ 8.1 (fL) | N/L ratio ≥ 4.1 | ||||
| Sensitivity | 67.2% | 54.0%-78.7% | 88.5% | 77.8%-95.3% | |
| Specificity | 72.7% | 62.9%-81.2% | 42.4% | 32.5%-52.8% | |
| DA | 70.6% | 62.9%-77.6% | 60.0% | 52.0%-67.7% | |
| Youden's index | 39.9% | 25.3%-54.6% | 30.9% | 18.3%-43.5% | |
| PPV | 60.3% | 47.7%-72.0% | 48.6% | 39.0%-58.3% | |
| NPV | 78.3% | 68.4%-86.2% | 85.7% | 72.8%-94.1% | |
| LR+ | 2.46 | 1.71-3.55 | 1.54 | 1.27-1.86 | |
| LR- | 0.45 | 0.31-0.66 | 0.27 | 0.13-0.56 | |
| LR | 5.47 | 2.73-10.94 | 5.68 | 2.35-13.74 | |
Tab. 4. Diagnostic characteristics of suggested cutoff points in diagnosing placenta accrete.
Receiver Operator Characteristics (ROC) curves (Tab. 5. & Fig. 2.) were constructed for laboratory data to predict placenta accreta in the women included. RDW%, Platelets, MPV, and N/L ratio indices were significant predictors as denoted by the significantly large Area Under the Curves (AUCs), with MPV being the most significant predictor.
| AUC | SE | 95% CI | p-value | |
|---|---|---|---|---|
| RDW (%) | 0.668 | 0.043 | 0.583-0.752 | <0.001* |
| Platelets | 0.635 | 0.044 | 0.549-0.721 | 0.004* |
| MPV | 0.780 | 0.036 | 0.709-0.850 | <0.001* |
| Lymphocyte | 0.535 | 0.048 | 0.441-0.628 | 0.462 |
| Neutrophils | 0.586 | 0.047 | 0.495-0.679 | 0.065 |
| N/L ratio | 0.696 | 0.043 | 0.611-0.780 | <0.001* |
| P/L ratio | 0.437 | 0.046 | 0.347-0.527 | 0.184 |
Tab. 5. Diagnostic performance of laboratory findings in diagnosing placenta accrete.
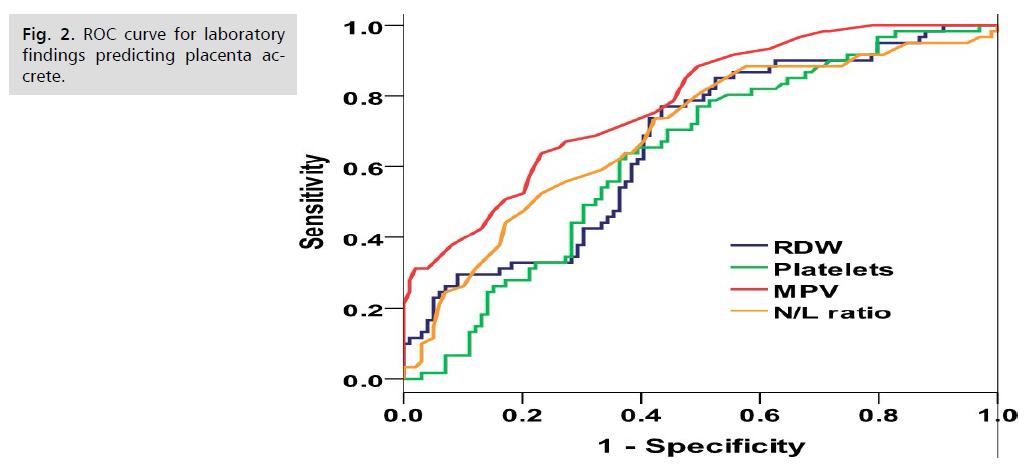
Fig 2. ROC curve for laboratory findings predicting placenta accrete.
Discussion
Our results and their interpretation
This study included 160 patients diagnosed with placenta previa and suspected placenta accrete spectrum. We studied the possible role of CBC parameters in the prediction of PAS. Our results showed no significant difference between the placenta previa and the accreta groups regarding the demographic data. Regarding the CBC parameters, there was a highly statistically significant difference between the previa and the accreta groups regarding Mean Platelet Volume (MPV). The two groups had a statistically significant difference regarding RDW, platelets, and Neutrophil/Platelet ratio. MPV and N/L were significantly higher in cases with placenta accreta; however, RDW and platelet counts were significantly lower in cases with placenta accreta. The ROC characteristics showed that RDW%, Platelets, MPV, and N/L ratio indices were significant predictors, as denoted by the significantly large Area Under the Curves (AUCs), with MPV being the most important predictor.
Excessive trophoblast invasion into the uterine decidua is found in cases of the Placenta accreta spectrum. Many researchers proved the same invasion behavior in cancer cells and trophoblasts and similarities in the proliferation and migration behavior. In the placenta accreta spectrum, Matrix metalloproteinases MMP-2 and MMP-9 are highly expressed. In cancer cells, the high expression of these metalloproteinases is linked to angiogenesis and invasion. There is increased expression of VEGF in both cancer cells and trophoblastic cells in PAS [7,8].
Several studies showed the association of systemic inflammatory markers (including neutrophil/lymphocyte ratio and platelet/lymphocyte ratio) in the pathogenesis of several gynecological cancers, such as endometrial and ovarian cancer [3,4,9].
Many studies have suggested that chronic inflammation cells play a role in tumor migration, proliferation, and survival. The decidual trophoblastic cells in PAS act in a similar way as malignant cells [10,11]
Comparison of the results of the current study with similar studies
Only a few studies have studied the role of CBC parameters in abnormal placentation; all were performed in Turkey, and three were retrospective [5,6,10,11]. In the retrospective study of Ersoy, et al. 2016 [5], they recruited 93 patients diagnosed with placenta previa and 247 controls. Total leukocyte count, neutrophil count, and N/L were significantly higher in the PP group; in our study, only the N/L ratio was higher due to differences in inclusion criteria and patient groups. The mean of MPV was significantly lower in their placenta previa group (10.48). Our study has a higher mean with a high statistically significant difference between the previa and accreta groups. Mean Platelet Volume (MPV) was significantly lower in the placenta previa group compared to controls, which agreed with our study.
In a prospective study by Abide Yayla, et al. 2017 [6] that included 146 patients with suspected placental accreta spectrum, CBC was done before CS. PAS was histopathologically confirmed in 46 cases, so there were two subgroups as in our study. There were significant differences between the two groups regarding neutrophil, platelet count, MPV, RDW, and neutrophil-to-lymphocyte ratio. Similar to our study except for neutrophil and platelet count, in which there was a difference but did not reach a statistically significant level.
In the retrospective case-control study of Karapinar, et al. [10], 70 cases with placenta previa and 70 control cases were recruited. As regards the CBC parameters, the MPV was significantly lower in the previous group. Placental accreta spectrum was confirmed in 24 cases. MPV was also significantly lower in the PAS group than in the control group (p=0.047). We attribute the difference in their results to the small number of studied patients.
In the retrospective case-control study of Ozgen and Ozgen 2020 [11], 181 women were recruited into three groups as follows: 77 patients with Placenta Previa (PP), 52 with confirmed Placenta Accreata Spectrum (PAS), and 52 women as control group. CBC parameters showed that neutrophils and N/L ratio were significantly higher in the previa and accreta groups. Similar to our study, the platelets were substantially lower in the Placenta Previa group. Also, by multivariate analyses, mean platelet volume (OR 4.01; 95% CI 2.4–6.6) was significantly associated with the placental accreta spectrum (p<0.001).
Strengths and Limitations of Our Study
The strength of our study is that only a few studies handled the parameters of CBC bias in the placenta accreta spectrum, and it was done in one of the biggest tertiary hospitals in Egypt, while the limitation of our study is that it is not multicentric study and this represents a significant risk of publication bias.
Recommendations for Further Research
Further studies are needed with large sample sizes and multicenter studies.
Conclusion
Besides the ultrasound and MRI findings, simple CBC is an inexpensive and reliable tool in screening the placenta accreta spectrum.
Consent for Publication
Non-applicable
Availability and Data Material
The datasets used and analyzed during the current study are available from the corresponding author upon reasonable request.
Competing Interests
The authors report there are no competing interests to declare
Funding
This study received no financial support.
References
- American College of Obstetricians and Gynecologists, Society for Maternal-Fetal Medicine. Obstetric care consensus no. 7: Placenta accreta spectrum. Obstet Gynecol. 2018;132(6):e259-275.
- Diag FP, Jauniaux E, Bhide A, et al. FIGO consensus guidelines on placenta accreta spectrum disorders: Prenatal diagnosis and screening. Int J Gynecol Obstet. 2018.
- Feng Z, Wen H, Bi R, et al. Preoperative neutrophil-to-lymphocyte ratio as a predictive and prognostic factor for high-grade serous ovarian cancer. PLoS One. 2016;11(5):e0156101.
- Akın MN, Kasap BH, Yuvacı HU. Neutrophil-to-lymphocyte ratio and platelet distribution in patients with endometrial cancer. J Obstet Gynaecol. 2015;41(9):1499.
- Ersoy AO, Ozler S, Oztas E, et al. The association between placenta previa and leukocyte and platelet indices—a case control study. Ginekol Pol. 2016;87(5):367-371.
- Abide Yayla C, Ozkaya E, Tayyar A, et al. Predictive value of complete blood count parameters for placental invasion anomalies. J Matern Fetal Neonatal Med. 2017;30(19):2324-2328.
- Krstic J, Deutsch A, Fuchs J, et al. (Dis) similarities between the Decidual and Tumor Microenvironment. Biomedicines. 2022;10(5):1065.
- Bartels HC, Postle JD, Downey P, et al. Placenta accreta spectrum: A review of pathology, molecular biology, and biomarkers. Dis Markers. 2018;2018.
- Kim HS, Han KH, Chung HH, et al. Neutrophil to lymphocyte ratio for preoperative diagnosis of uterine sarcomas: A case-matched comparison. Eur J Surg Oncol. 2010;36(7):691-698.
- Karapınar OS, Gözükara I, Hakverdi AU, et al. A new marker for the prediction of mean platelet volume, placenta previa and placental invasion anomalies. J Matern Fetal Neonatal Med. 2017;25(1):32-37.
- Özgen G, Özgen L. Complete blood count parameters in the antepartum diagnosis of placental invasion anomalies. Ann Clin Anal Med. 2020;11(6):592-597.
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Author Info
Ahmed Sherif Abd El Hamid*, Abd El Megeed Ismail Abd El Megeed, Rawhia Elsayed Mohammed Elsayed and Ahmed Mahmoud HusseinCopyright:This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.