Research - (2025) Volume 20, Issue 1
Effect of iron overload on inhibin B synthesis in transfusion dependent Thalassemic women
Dina A.A.Abdullah1, Fatimah Kadhim Ibrahim AL-Mahdawi2*, Mazin Razooqi Mohammed3, Ammar Kadi4, Marouane Chemek4 and Irina Potoroko4Received: 25-Jan-2025, Manuscript No. gpmp-25-160120; Editor assigned: 27-Jan-2025, Pre QC No. P-160120; Reviewed: 11-Feb-2025, QC No. Q-160120; Revised: 28-Feb-2025, Manuscript No. R-160120; Published: 31-Mar-2025
Abstract
In women with thalassemia, particularly those with beta-thalassemia major, levels of inhibin B can be decreased, especially in those with significant iron overload, and there can be damage to the Gonads (testes in males, ovaries in females). This study was designed to determine inhibin B levels. In women with thalassemia undergoing regular blood transfusions, 40 female patients were included in this study was transfusion-dependent beta-thalassemia, with an age range of 18–20 years. All patients received blood transfusions at regular intervals (once/ month) to maintain a hemoglobin level of at least 10 gm/dl, all patients included in this study did not take iron Chelating therapy and have ferritin level >4000 µg/L. A hormone assay was done with hormones using the COBAS e411 test (from Roche, company). They used ELISA to test for Inhibin B and did a statistical analysis that showed pituitary hormones dropped significantly in thalassemic women compared to healthy women (p-value <0.001) and ovarian hormones dropped significantly in thalassemic women compared to healthy women (p-value <0.00). Iron overload is transfusion-dependent. Thalassemia is often linked to several endocrine problems that throw off the body's hormones and ovaries. This can make it harder to get pregnant, so it's important to keep this patient's iron levels in check with the right iron-checking therapy.
Keywords
Thalassemic women; Inhibin B; Iron over load; Iron chelating
Introduction
Inhibin B is a glycoprotein hormone that plays an important role in the regulation of the hypothalamic-pituitary-gonadal axis. It is mostly made by the Sertoli cells in males and the granulosa cells in females. In males, it shows that spermatogenesis is happening, and in females, it shows that the ovarian reserve is full [1,2]. People who have thalassemia, a group of inherited blood disorders where the body doesn't make enough hemoglobin or doesn't make any at all, can develop a number of systemic problems, such as endocrine problems [3]. Patients with thalassemia, particularly those with beta-thalassemia major, often suffer from iron overload due to frequent blood transfusions and increased intestinal iron absorption [4]. This iron overload can deposit in various organs, including the endocrine glands, leading to dysfunction [5]. In women with thalassemia, particularly those with beta-thalassemia major, levels of inhibin B can be decreased. Specifically, the granulosa cells of the ovaries make the hormone inhibin B. This hormone is very important for controlling the menstrual cycle and fertility because it stops the pituitary gland from releasing follicle-stimulating hormone (FSH). In thalassemia patients, especially those with significant iron overload, there can be damage to the gonads (testes in males, ovaries in females) [6,7]. This can lead to less inhibin B being made because the Sertoli cells in males and the granulosa cells in females don't work as well. Lower levels of inhibin B may be observed, indicating compromised gonadal function [8]. Therefore, this study was designed to determine inhibin B levels in women with thalassemia undergoing regular blood transfusions.
Materials and Methods
Subjects
40 female patients were included in this study transfusion-dependent beta-thalassemia, with an age range of 18-20 years. All patients received blood transfusions at regular intervals (once/month) to maintain a hemoglobin level of at least 10 gm/dl. All patients included in this study did not take iron-chelating therapy and had ferritin levels >4000 µg/L.
Inclusion criteria: The study focused on women with transfusion-dependent thalassemia major, with an age range of 18-20 years.
Exclusion criteria: The patients are on iron-chelating therapy. Patients undergoing a splenectomy
Methods
Aseptic techniques were used to get 4 ml of venous blood from 40 women who volunteered for this study on the second day of their period. The blood was then put into a gel tube container that was used for the COBAS e411 test (from Roche), which measured parameters and hormones. While inhibin B assessment was done by ELISA techniques.
Statistical analysis of all data was done by using a t-test. A p value less than 0.05 was regarded as significant differences.
Results
The pituitary hormones illustrated in Tab. 1., the LH, FSH, and prolactin within normal range (1.6-12.4IU/L, 1.20-12.50IU/L, and 3.00-23.00ng/ml respectively) in thalassemic women (2.86 ± 0.04IU/L, 4.41 ± 0.07IU/L, and 8.00 ± 0.01ng/ml respectively), also in healthy women (7.15 ± 0.15IU/L, 7.98 ± 0.12IU/L, and 13.69 ± 0.11ng/ml respectively), the statistical analysis found the pituitary hormones decrease significantly in thalassemic women when compared with healthy women p-value <0.001 (Fig. 1.).
| Hormones | Normal range | Healthy Women Mean ± SE |
Thalassemic Women Mean ± SE |
t-test p-value |
|---|---|---|---|---|
| LH IU/L | 1.6-12.4 | 7.15 ± 0.15 | 2.86 ± 0.04 | 0.000 |
| FSH IU/L | 1.20-12.50 | 7.98 ± 0.12 | 4.41 ± 0.07 | 0.000 |
| Prolactin ng/ml | 3.00-23.00 | 13.69 ± 0.11 | 8.00 ± 0.01 | 0.000 |
Tab. 1. Pituitary hormone.
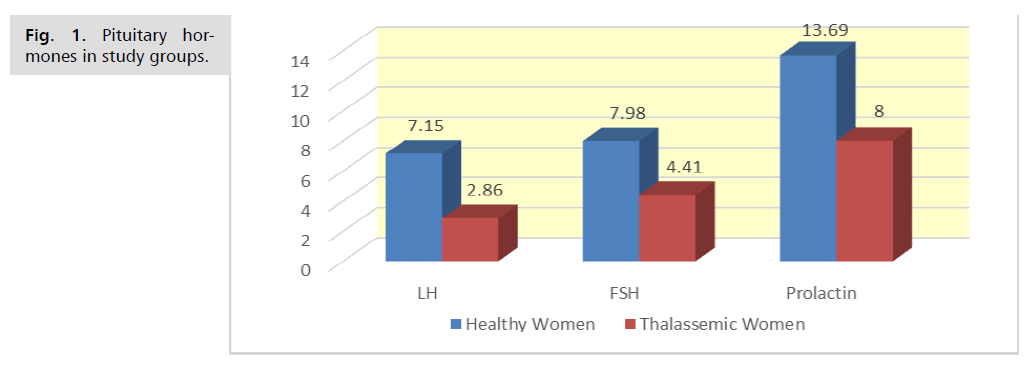
Fig. 1. Pituitary hormones in study groups.
The ovarian hormones illustrated in Tab. 2., the estradiol within the normal range (30.0-170.0 pg/ml) in thalassemic women (35.98 ± 1.22 pg/ml) and in healthy women (86.16 ± 0.76 pg/ml), while testosterone, and inhibin b hormones less than the normal range (0.06-0.40ng/ml, and Up to 17 pg/ml) in thalassemic women (0.02 ± 0.04 ng/ml, and 3.68 ± 0.13 pg/ml), while within normal range in healthy women (0.27 ± 0.01 ng/ml, and 28.24 ± 0.34 pg/ml), the statistical analysis found the ovarian hormones decrease significantly in thalassemic women when compared with healthy women p-value <0.001 (Fig. 2.).
| Hormones | Normal range | Healthy Women Mean ± SE |
Thalassemic Women Mean ± SE |
t-test p-value |
|---|---|---|---|---|
| Estradiol pg/ml | 30.0-170.0 | 86.16 ± 0.76 | 35.98 ± 1.22 | 0.000 |
| Testosterone ng/ml | 0.06-0.40 | 0.27 ± 0.01 | 0.02 ± 0.04 | 0.000 |
| Inhibin b pg/ml | Up to 17 | 28.24 ± 0.34 | 3.68 ± 0.13 | 0.000 |
Tab. 2. Ovarian hormone.
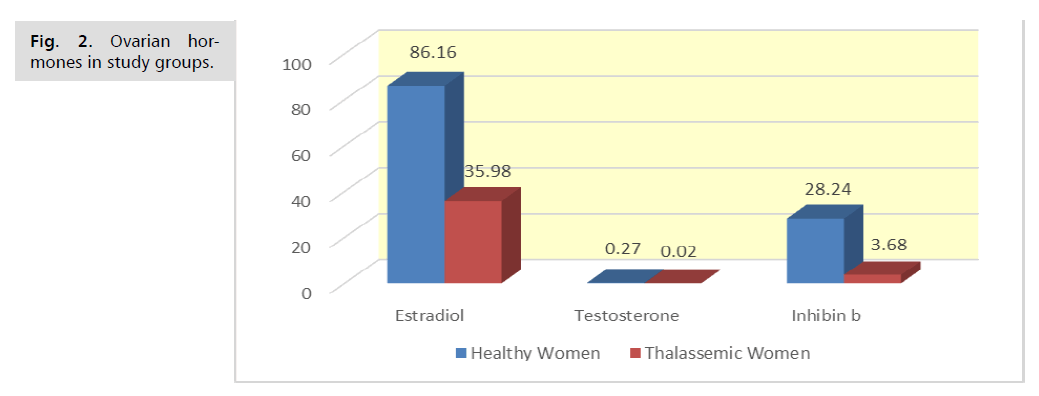
Fig. 2. Ovarian hormones in study groups.
Discussion
Women with B-thalassemia major, particularly those with regular blood transfusions, commonly develop decreased secretion of ovarian hormones LH and FSH [9,10]. This hormonal imbalance often leads to delayed puberty, menstrual irregularities, and infertility [11]. Thalassemia patients often undergo regular blood transfusions, causing accumulation of iron in different tissues, particularly the pituitary gland, which is responsible for producing LH and FSH. Iron deposition in the pituitary gland can impair its function, reducing the secretion of these hormones [12].
In this study, we confirmed the fact that endocrine abnormalities in the study group were related to iron deposits in the pituitary gland. So patients have a lower level of FSH, LH, and low sex steroids [9].
The condition of iron-induced destruction to the endocrine tissues often results in hypogonadotropic hypogonadism. This means that the hypothalamus or pituitary gland fails to produce sufficient levels of GnRH or gonadotropins (LH and FSH), respectively [13,14].
In this finding, inhibin B decreases significantly in thalassemic women. The decrease in inhibin B levels in thalassemic women can be attributed to several factors, including iron overload and ovarian damage. Frequent blood transfusions in thalassemia patients often lead to excessive iron accumulation in the organs and tissues [15]. This accumulation extends to the ovaries, leading to oxidative stress and cellular damage. This can make ovarian granulosa cells less effective, which lowers the production of inhibin B [16]. Also, iron overload can damage the pituitary gland, leading to insufficient production of gonadotropins (LH and FSH). Lower FSH levels can make it harder for ovarian follicles to grow and work properly, which can cause granulosa cells to make less inhibin B [15,17]. Iron toxicity may also cause a premature decline in ovarian reserve in women with thalassemia. Less ovarian reserve means fewer follicles and granulosa cells that can work, which lowers the amount of inhibin B in the body [18-20].
Conclusion
Iron overload is transfusion-dependent. Thalassemia is often associated with multiple endocrine abnormalities, affecting the overall hormonal balance and ovarian function, which in turn leads to reduced fertility, so it’s mandatory to control iron status in this patient through the appropriate use of iron chelating therapy.
Author Contributions
Conceptualization, F.M., M.M., M.C., A.K., and I.P.; original draft preparation, F.M. and M.M.; writing—review and editing F.M., M.M., M.C., A.K. and I.P. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare that there are no conflicts of interest.
References
- Jin JM, Yang WX. Molecular regulation of hypothalamus–pituitary–gonads axis in males. Gene. 2014;551(1):15-25.
- Al-Obaidy EN, Al-Samarrai AM. Relationship of Inhibin-B with Gonadal Hormones Levels in Seminal Plasma of Infertile Patients in Diyala Governorate. Iraqi J Embryos Infertil Res. 2017;7(1):1.
- Mohammed MR, Hamoode RH, Al-Mahdawi FK. Hypoparathyroidism due to iron overload in beta-thalassemia patients. Biomed. 2022;42(6):1305-1308.
- AL-Mahdawi FK, Mohammed MR, Mahmood MM. Screening tests for voluntarily donated blood in Diyala governorate. In AIP Conference Proceedings 2022 (Vol. 2398, No. 1). AIP Publishing.
- Surbek DV, Holzgreve W. Infertility in β-thalassemia major. Am J Obstet Gynecol. 1996;175(4):1080-1081.
- Sinharay M, Mitra S, Dasgupta A. Effect of iron overload on gonadotrophins and organ sex steroids in pubertal thalassemia patients. Int J Cur Res Rev. 2017;9(23):15-21.
- Elia ZN, AL-Mahdawi FK, Berwary NJ. Estimation of Anti-thyroglobulin and Anti-Thyroid peroxidase among thalassemia major patients. Ann Trop Med Public Health. 2019;22:12.
- De Sanctis V, Giovannini M. Endocrine histology findings in a prepubertal thalassemic girl with multiple endocrine complications secondary to iron overload. Georgian Med News. 2011;193:51-55.
- Singer ST, Sweeters N, Vega O, et al. Fertility potential in thalassemia major women: current findings and future diagnostic tools. Ann N Y Acad Sci. 2010;1202(1):226-230.
- Uysal A, Alkan G, Kurtoğlu A, et al. Diminished ovarian reserve in women with transfusion-dependent beta-thalassemia major: Is iron gonadotoxic?. Eur J Obstet Gynecol Reprod Biol. 2017;216:69-73.
- Casale M, Baldini MI, Del Monte P, et al. Good clinical practice of the Italian Society of Thalassemia and Haemoglobinopathies (SITE) for the management of endocrine complications in patients with haemoglobinopathies. J Clin Med. 2022;11(7):1826.
- Macchi C, Steffani L, Oleari R, et al. Iron overload induces hypogonadism in male mice via extrahypothalamic mechanisms. Mol Cell Endocrinol. 2017;454:135-145.
- Zhang J, Su T, Fan Y, et al. Spotlight on iron overload and ferroptosis: Research progress in female infertility. Life Sci. 2024;340:122370.
- Chang HH, Chen MJ, Lu MY, et al. Iron overload is associated with low anti‐müllerian hormone in women with transfusion‐dependent β‐thalassaemia. BJOG. 2011;118(7):825-831.
- Singer ST, Vichinsky EP, Gildengorin G, et al. Reproductive capacity in iron overloaded women with thalassemia major. Blood. 2011;118(10):2878-2881.
- Rossi EM, Marques VB, Nunes DD, et al. Acute iron overload leads to hypothalamic-pituitary-gonadal axis abnormalities in female rats. Toxicol Lett. 2016;240(1):196-213.
- Mousa AA, Ghonem M, Elhadidy EH, et al. Iron overload detection using pituitary and hepatic MRI in thalassemic patients having short stature and hypogonadism. Endocr Res. 2016;41(2):81-88.
- Kobayashi H, Yamada Y, Kanayama S, et al. The role of iron in the pathogenesis of endometriosis. Gynecol Endocrinol. 2009;25(1):39-52.
- Ibrahim AL-Mahdawi FK, Elia ZN, Kurji HA. Evaluation Inhibin B, FSH, and LH in Male with Thalassemia. Indian J Forensic Med Toxicol. 2020;14(2).
- Donnelly P, Tan K, Winch D. Inhibin B levels in hypothyroid males. Thyroid. 2013 ;23(11):1379-82.
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Author Info
Dina A.A.Abdullah1, Fatimah Kadhim Ibrahim AL-Mahdawi2*, Mazin Razooqi Mohammed3, Ammar Kadi4, Marouane Chemek4 and Irina Potoroko42College of Dentistry, university of diyala, Diyala, Iraq
3Bilad Alrafidain University College, Diyala, Iraq
4Department of Food and Biotechnology, South Ural State University, Chelyabinsk, Russia
Copyright:This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.