Research - (2025) Volume 20, Issue 2
Assessing warm saline's role in alleviating pain in office hysteroscopy: A systematic review and meta-analysis
Mohammed Abdelrazeq#, Salwa Neyazi1, Khalid Akkour1, Nada Alayed1, Omar Alzaydan1, Eman Al Shehri1, Shadan Binsaeedan1, Ahmed Sherif1,2*, Alhassan Khedr2, Sondos Al Hawamdeh3, Mohammed Alatawi4, Mohammad Atlam5,6, Munirah Mohammed Binmosa1 and Karim Abdelsalam7Received: 21-Apr-2025, Manuscript No. gpmp-25-16458; Editor assigned: 23-Apr-2025, Pre QC No. P-16458; Reviewed: 05-May-2025, QC No. Q-16458; Revised: 23-Jun-2025 Published: 30-Jun-2025
Abstract
Background: This systematic review and meta-analysis evaluated the effectiveness of using warm saline as a distension medium compared to room temperature saline in reducing pain and improving patient satisfaction during office hysteroscopy. Methodology: Following PRISMA guidelines and registered in PROSPERO (CRD420251074073), we systematically searched MEDLINE, Scopus, Web of Science, and Cochrane Central for RCTs from inception to June 2025. Our search combined MeSH terms and keywords related to hysteroscopy, distension media, and pain management. We included RCTs that compared warm and room temperature saline in women undergoing diagnostic or operative office hysteroscopy. Two authors independently extracted data and assessed the risk of bias using the Cochrane Risk of Bias tool. Continuous outcomes were pooled as mean differences (MD) and dichotomous outcomes as odds ratios (OR) with 95% confidence intervals (CI) using RevMan software. Heterogeneity was assessed using the I² statistic, and sensitivity analyses were conducted to address variability. Results: Our meta-analysis included seven RCTs with a total of 541 women. Warm saline significantly reduced pain during the procedure, with a mean difference of -0.92 (95% CI: -1.50 to -0.34, p=0.002), despite high heterogeneity (I² = 83%). Post-procedure pain also significantly decreased, with a mean difference of -0.47 (95% CI: -0.79,-0.150, p = 0.004), and heterogeneity was substantial (I² = 67%). Patient satisfaction was significantly higher with warmed saline, with an odds ratio of 2.70 (95% CI: 1.49 to 4.91, p=0.001), although heterogeneity remained moderate (I² = 44%). Conclusion: Warm saline as a distension medium during office hysteroscopy significantly reduces procedural pain and enhances patient satisfaction. These findings support the adoption of warm saline to improve patient experience and compliance, promoting a more patientcentered approach in gynecological care.
Keywords
Warm saline: Pain; Hysteroscopy
Introduction
Office hysteroscopy is a minimally invasive procedure that uses a thin tube and camera to examine the inside of the uterus without the need for incisions or anesthesia. It serves as an effective diagnostic tool for identifying conditions such as abnormal uterine bleeding, polyps, and intrauterine devices, as well as for performing treatments like polypectomy and endometrial ablation. The procedure provides clear visualization of the uterine cavity, making it a preferred method for outpatient gynecological assessments [1].
During hysteroscopy, the uterine cavity is distended with saline or carbon dioxide gas to improve visibility. Saline is commonly used because it is effective and associated with fewer vasovagal reactions. Maintaining a pressure of around 40 mm Hg ensures proper distension and visualization. To reduce discomfort, various pain management strategies are employed, including pharmacological methods like NSAIDs and nerve blocks, as well as nonpharmacological approaches such as using smaller hysteroscopes or specialized techniques [2-4].
The temperature of the distension saline—whether warmed or at room temperature—may influence patient comfort, uterine contractions, and overall satisfaction. It is hypothesized that warm saline could reduce pain and improve procedural outcomes by minimizing uterine spasms. However, there is limited research on how temperature affects pain, image clarity, or patient satisfaction, highlighting the need for further studies to determine its clinical significance in outpatient hysteroscopy [5-7].
There is conflicting evidence regarding how the temperature of the distension fluid affects pain during office hysteroscopy. Several studies found that using warm saline significantly reduces pain during and after the procedure [1, 7-9]. At the same time, another study [6, 10-11] et al. reported no significant difference between warm and room temperature saline in pain relief. To clarify these discrepancies, we conducted a systematic review and meta-analysis to evaluate whether warm saline as a distension medium effectively reduces pain in outpatient hysteroscopy [8-9].
Protocol, Search Strategies, and Sources
This systematic review followed PRISMA guidelines [12] and was registered in PROSPERO in 2025 (CRD420251074073). Two authors (Salwa Neyazi, Khalid Akkour) systematically searched MEDLINE, Scopus, Web of Science, and Cochrane Central for randomized controlled trials (RCTs) examining the effects of distension fluid temperature on pain during office hysteroscopy, from inception to June 2025, with no language restrictions. Additionally, they reviewed references of relevant studies and articles. Our search combined Medical Subject Headings (MeSH) terms, key search words, (hysteroscopy OR endoscopy, hysteroscopic OR hysteroscopic procedure) AND (distension media OR saline infusion OR fluid infusion OR distension fluid OR saline OR normal saline OR distension medium OR distension media) AND (warm OR temperature OR heated OR thermal OR room temperature OR temperature-controlled OR cold) AND (pain management OR discomfort OR procedural pain OR pain relief OR analgesia OR pain control) AND (outpatient OR office-based OR ambulatory OR outpatient hysteroscopy OR office hysteroscopy).
Screening and Study Selection
Two review authors, Shadan Binsaeedan and Sondos Al Hawamdeh, utilized a reference management tool to import search results and remove duplicates. They independently screened the titles and abstracts of the retrieved studies for potential eligibility for full-text review. Subsequently, Eman Al Shehri and Mohammed AbdelRazeq double-checked the list of studies flagged as potentially eligible to ensure accuracy and completeness. Nada Alayed and Omar Zidan performed title, abstract, and full-text screening, reaching consensus through discussion. Irrelevant studies, reviews, unpublished, non-randomized, or abstract-only only were excluded. Any disagreements during this process were resolved through discussion and consultation with a third author, Mohammed Alatawi. A PRISMA flowchart visually summarizes the selection process, illustrating each step from initial identification to final inclusion.
Data Collection and Outcomes
Two authors (Mohammed Alatawi and Mohammad Atlam) independently extracted data from the included trials using a standardized form, assessing each study's eligibility and quality. Any disagreements were resolved by a third author (Ahmed Sherif). We included RCTs where warm saline was used as the distension medium in the intervention group, compared to room temperature saline in the control group, among women undergoing hysteroscopy for various reasons. Our primary outcomes were pain scores evaluated during and after office hysteroscopy procedure using the visual analog scale (VAS). Our secondary outcome was satisfaction, in which we assessed the number of patients who were satisfied with the procedure among both groups.
Risk of Bias
Two authors (Salwa Neyazi and Khalid Akkour) independently assessed the risk of bias in the included studies using the Cochrane Risk of Bias tool [13], evaluating domains such as random sequence generation, allocation concealment, performance bias (blinding of participants and personnel), detection bias (blinding of outcome assessment), attrition bias, reporting bias, and other biases. Discrepancies were resolved through discussion to reach consensus; any disagreement was solved by the primary author (Ahmed Sherif). Each domain was rated as unclear, high, or low risk. This evaluation was crucial for interpreting the reliability of the findings and understanding potential sources of heterogeneity.
Measures of Effect
Data from the included trials were analyzed following the Cochrane Handbook guidelines [12]. Both continuous and dichotomous outcomes were pooled as mean differences (MD) and odds ratios (OR) with 95% confidence intervals (CI). Data analysis was performed using RevMan software by two authors (Eman Al Shehri and Nada Alayed), with a third author (Ahmed Sherif) consulted when disagreements arose. A random-effects model was used in cases of heterogeneity, while a fixed-effect model was employed when heterogeneity was low. The I2 statistic assessed heterogeneity, with values ≥50% indicating high heterogeneity. Sensitivity analyses were conducted to address heterogeneity. Continuous data were pooled as mean differences, and dichotomous data as odds ratios, ensuring comprehensive analysis despite incomplete datasets. This approach helped maintain the integrity of the meta-analysis and supported accurate effect estimates.
Assessment of Heterogeneity
The I2 statistic evaluated study heterogeneity. 50% or higher values indicated significant heterogeneity, prompting subgroup analyses to explore potential sources. When heterogeneity was present, a random-effects model was applied to account for variability across studies. For low heterogeneity, a fixed-effect model synthesized the results.
Assessment of Publication Bias
Funnel plots and Egger’s test [14-15] were planned to assess publication bias. However, with fewer than 10 studies included, these tests were unreliable, and publication bias could not be conclusively evaluated [16]. Consequently, the small number of RCTs limited the assessment of potential bias in the meta-analysis.
Results
The PRISMA flowchart outlines the systematic review process, beginning with 55 records identified through database searching. After removing duplicates, 35 records were screened based on titles and abstracts, leading to 13 full-text articles assessed for eligibility. Of these, six full texts were excluded—five due to irrelevance and one for being abstract-only, leaving seven studies included in the meta-analysis (Fig. 1. & Tab. 1.).
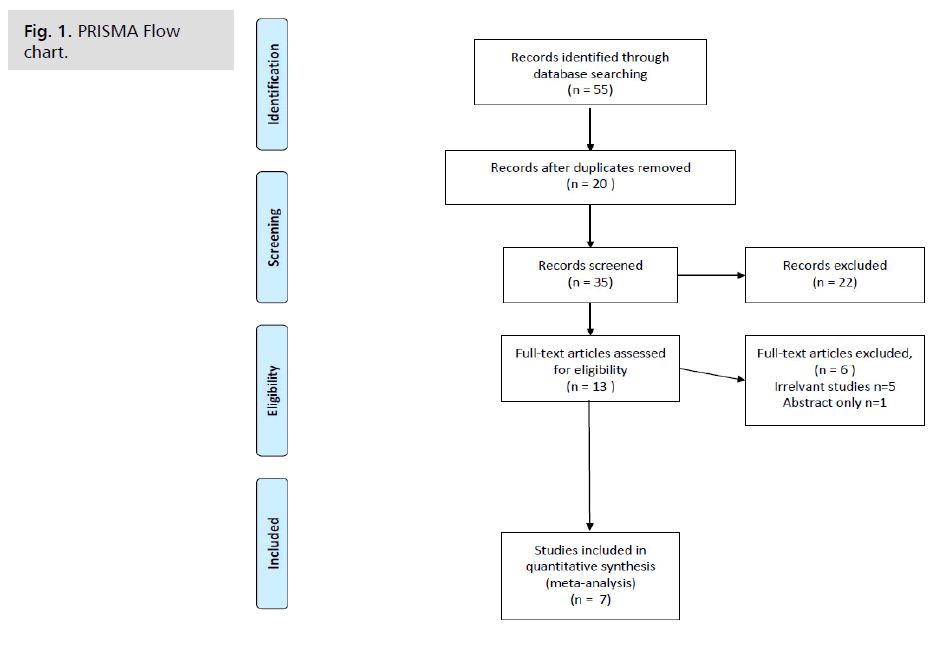
Fig. 1. PRISMA Flow chart.
| Study name | Population | Intervention | Comparison | Outcome | Results |
|---|---|---|---|---|---|
| Gulucu and Cakmak 2021 [7] | Perimenopausal Women undergoing office hysteroscopy | Warm saline application n=50 | Normal saline group n=49 | Pain score VAS | The VAS scores were significantly lower for patients in the warm fluid group than in the room temperature group (P<.05), |
| Evangelista et al. 2011 | Women undergoing hysteroscopy | Warm saline application n=34 | Normal saline group n=30 | Pain score and satisfaction score | There were no significant differences in pain intensity immediately after the examination (p = 0.51), at 1 minute (p = 0.96), or at 15 minutes (p = 0.96), and the satisfaction rate with the warmed distention medium was similar to that of the room-temperature saline solution (p = 0.48). |
| Kapur et al. 2020 [6] | Outpatient hysteroscopy for AUB, removal of IUCD, and excision of endometrial polyps. | Warm saline application n=52 | Normal saline group n=48 | procedure duration, ease of entry, view clarity, pain during and after hysteroscopy, and satisfaction | No significant differences in procedure duration, ease of entry, view clarity, discomfort, or recommendation likelihood between groups (all P > 0.05). |
| Nair et al. 2020 [8] | Women undergoing office hysteroscopy | Warm saline application n=55 | Room temperature saline group n=55 | VAS pain scores , patient satisfaction | The VAS scores were significantly lower for patients in the warm fluid group than in the room temperature group (P=0.001), higher satisfaction (P=0.001) |
| Tawfek et al. 2019 [9] | Women undergoing office hysteroscopy | Warm saline application n=41 | Room temperature saline group n=41 | VAS pain scores , patient satisfaction | pain scores was significantly reduced in the warm saline group both during and after the procedure (p < 0.001). Additionally, patient satisfaction was higher in the warm saline group, p < 0.04) |
| Sharma et al 2022 [11] | Women undergoing office hysteroscopy | Warm saline application n=50 | Room temperature saline group n=50 | The study found no significant differences between in VAS scores or satisfaction between groups p>0.05 | |
| Ahmed et al.2024 [1] | Women undergoing office hysteroscopy | Warm saline application n=48 | Room temperature saline group n=49 | VAS pain scores , patient satisfaction | significant reduction in pain scores at the end of the procedure in the warm saline group (p = 0.002), while there was no significant difference in pain scores 15 minutes P>0.05, Satisfaction level is significantly higher p = 0.009 |
Tab. 1. Studies involved in the analysis, including PICO and main results.
Fig. 2. presents the risk of bias assessment for the included studies. Most studies exhibit a low risk across domains such as random sequence generation, allocation concealment, blinding of participants and personnel, outcome assessment, incomplete data, and reporting bias. However, studies of Kapur et al. [6] and Nair et al. [8] have uncleared risks in areas like allocation concealment and blinding, which may introduce bias. The assessment indicates a relatively high risk of selection, performance, and detection biases due to limited blinding in several studies. This potential bias could impact the validity of the findings, emphasizing cautious interpretation of the review results.
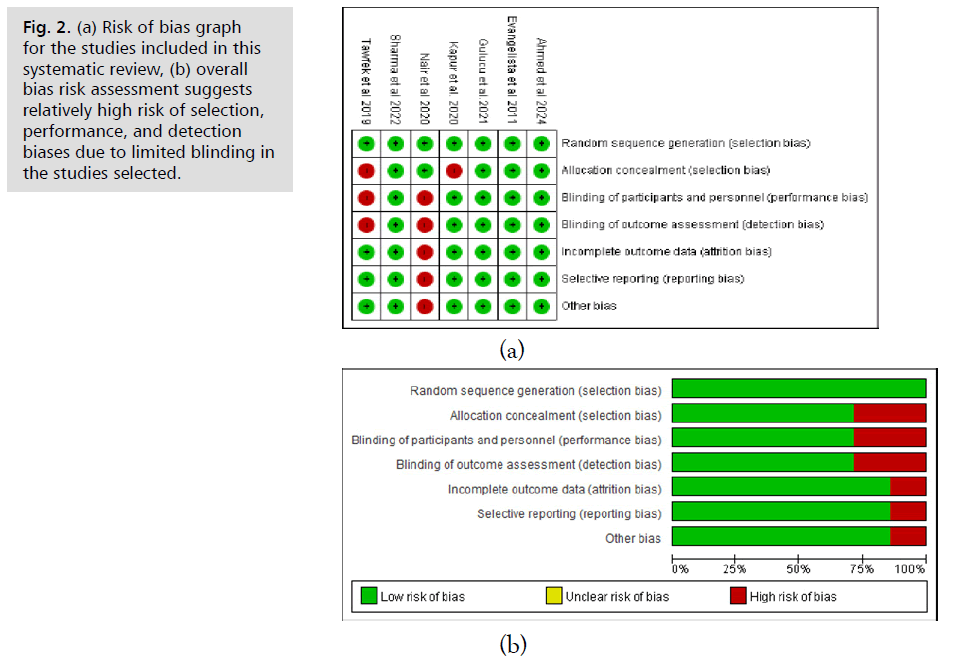
Fig. 2. (a) Risk of bias graph for the studies included in this systematic review, (b) overall bias risk assessment suggests relatively high risk of selection, performance, and detection biases due to limited blinding in the studies selected.
Fig. 3. compares warm saline (experimental group) versus room-temperature saline (control group) in reducing pain during the procedure. The overall mean difference is -0.92 (95% CI: -1.50 to -0.34, p=0.002), favoring warm saline, indicating it significantly reduces pain compared to room-temperature saline. However, heterogeneity is high (I2 = 83%), suggesting substantial variability among the included studies, possibly due to differences in patient populations, saline temperatures, or measurement methods.
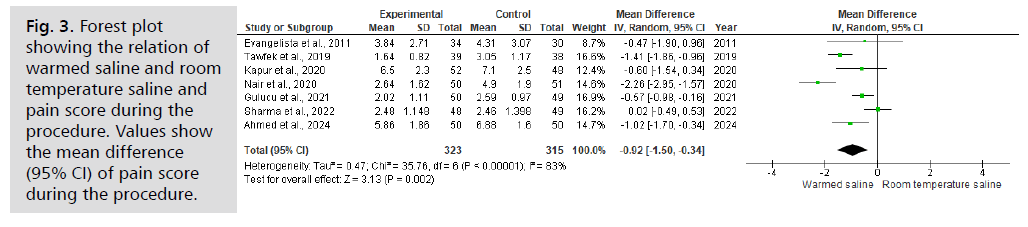
Fig. 3. Forest plot showing the relation of warmed saline and room temperature saline and pain score during the procedure. Values show the mean difference (95% CI) of pain score during the procedure.
Fig. 4. compares warmed saline and room temperature saline in terms of pain scores after the procedure. The overall mean difference is -0.47 (95% CI: -0.79,-0.150, p=0.004), favoring warmed saline, indicating it significantly reduces pain. The individual studies mostly show a trend toward lower pain scores with warmed saline, though some have wider confidence intervals crossing zero, indicating less certainty. The heterogeneity is high (I2 = 67%), suggesting substantial variability among studies, possibly due to differences in study design or patient populations. Despite the significant overall effect, the high heterogeneity suggests that results should be interpreted cautiously, and further research may be needed to confirm consistency across different settings.
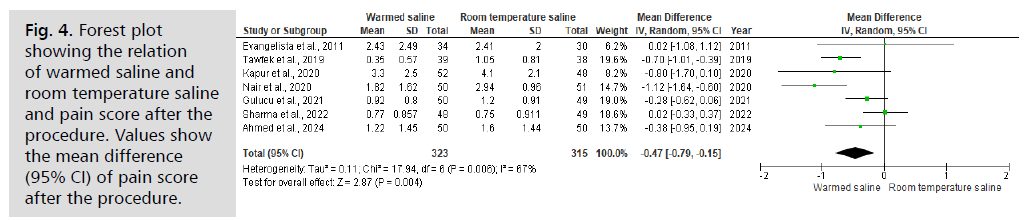
Fig. 4. Forest plot showing the relation of warmed saline and room temperature saline and pain score after the procedure. Values show the mean difference (95% CI) of pain score after the procedure.
The forest plot in Fig. 5. compares satisfaction levels between warmed saline and room temperature saline, with results expressed as odds ratios (OR) using a random-effects model. The combined OR is 2.70 (95% CI: 1.49 to 4.91), indicating that patients are significantly more likely to report satisfaction with warmed saline. Most individual studies favor warmed saline, although some have wider confidence intervals crossing the line of no effect. The heterogeneity is moderate (I2 = 44%), suggesting some variability among studies but consistent findings. The significant OR supports the conclusion that warmed saline improves patient satisfaction during the procedure, though the variability indicates further research may be beneficial.
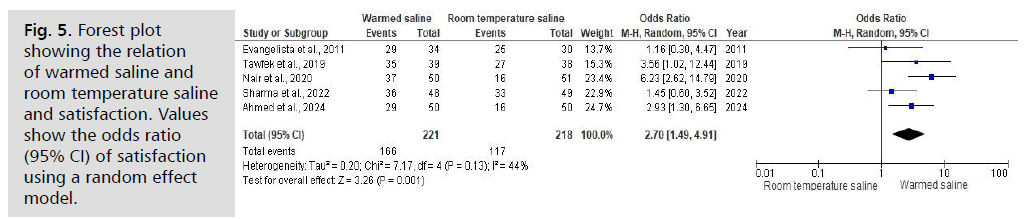
Fig. 5. Forest plot showing the relation of warmed saline and room temperature saline and satisfaction. Values show the odds ratio (95% CI) of satisfaction using a random effect model.
Overall, these findings highlight that warming distension fluid is a simple, cost-effective strategy to enhance patient comfort and satisfaction. The consistent reduction in pain during and after the procedure, along with increased satisfaction, underscores its potential to improve clinical outcomes and patient-centered care. While some heterogeneity suggests variability across studies, the robustness of the results after sensitivity analyses suggests that implementing warmed saline could be beneficial in routine practice, pending further standardized research to confirm these benefits across diverse settings.
Discussion
Our results and their interpretation
During the procedure, the results indicate that warmed saline significantly reduces pain, with a mean difference of -0.92 (95% CI: -1.50 to -0.34, p=0.002). Despite this positive finding, high heterogeneity (I2 = 83%) suggests considerable variability among studies, likely due to differences in patient characteristics, saline temperatures, or pain assessment methods. This variability warrants cautious interpretation, but overall, warm saline effectively minimizes pain during the procedure, enhancing patient comfort and cooperation. By improving patient comfort, warm saline could encourage more women to undergo necessary diagnostic and therapeutic procedures, ultimately enhancing healthcare outcomes.
Post-procedure pain scores also favor warmed saline, with a mean difference of -0.92 (95% CI: -1.50 to -0.34, p=0.002), indicating a significant reduction in pain after the procedure. However, heterogeneity remains high (I2 = 67%), reflecting differences in study designs or populations that may influence pain perception over time. While the trend supports the use of warmed saline for ongoing pain relief, the variability suggests that individual factors or procedural protocols could affect outcomes. Clinicians should consider these nuances when adopting warm saline, tailoring its use to patient-specific factors to maximize comfort.
Regarding patient satisfaction, the pooled odds ratio of 2.70 (95% CI: 1.49 to 4.91) shows that patients are significantly more satisfied with warmed saline during the procedure. Most studies favor warmed saline, though some have wider confidence intervals crossing the no-effect line, indicating variability in satisfaction levels. The moderate heterogeneity (I2 = 44%) suggests that while the overall trend is positive, differences in study settings or patient populations contribute to variability. These findings support the clinical advantage of warmed saline in improving patient satisfaction, but additional research could help refine protocols to optimize outcomes across diverse settings. These results advocate for the routine use of warm saline in office hysteroscopy, as it reduces pain and enhances patient satisfaction, ultimately fostering a more patient-centered approach to gynecological care.
Comparison of Our Results to Similar Reviews
Our review and the study by Craciunas et al. [17] highlight the advantages of using normal saline over other distension media, such as carbon dioxide, during hysteroscopy. While Craciunas et al. focused on comparing CO2 with normal saline, finding CO2 associated with greater procedural pain and less satisfaction, our review specifically examined the temperature of saline. We found that warm saline significantly reduced procedural pain and improved patient satisfaction. Both studies support using saline for better patient outcomes, though our review adds that warming saline can further enhance pain relief and satisfaction.
Our review corroborates the findings of Baradwan et al. [18] as both studies demonstrate that warm saline significantly reduces pain during and after hysteroscopy, with our meta-analysis showing a larger overall effect size during the procedure compared to the study of Baradwan et al. Similarly, post-procedure pain reduction is confirmed by both analyses. Regarding satisfaction, both studies report a significant increase with warmed saline, with our OR of 2.70 (95% CI: 1.49 to 4.91) compared to the previous OR of 3.71. Overall, both sets of findings support the beneficial effects of warmed saline, with our study indicating a potentially more potent impact, possibly due to differences in study inclusion or measurement methods.
Our study aligns with Silva et al. [19], showing that warming saline significantly reduces pain during and after hysteroscopy. Both studies found that saline as a distension medium improves patient satisfaction, with our OR of 2.70 supporting Silva et al.’s higher satisfaction scores with normal saline. While Silva et al. reported that warming saline did not reduce intraprocedural pain, our findings demonstrate a significant reduction, emphasizing that temperature modifications can further enhance patient comfort. Overall, both studies reinforce that saline, particularly warmed, optimizes pain management and satisfaction during hysteroscopy.
The clinical implications of this review are substantial. Using warm saline during office hysteroscopy significantly reduces procedural pain and enhances patient satisfaction. This simple intervention could lead to better patient compliance, increased willingness to undergo necessary diagnostic and therapeutic procedures, and improved patient outcomes. By adopting warm saline as a standard practice, healthcare providers can offer a more comfortable and positive experience, potentially reducing the anxiety and reluctance associated with gynecological procedures. This patient-centered approach improves individual care and promotes broader acceptance and utilization of office hysteroscopy in clinical settings.
Strengths and Limitations
This review's strengths include adherence to PRISMA guidelines, registration in PROSPERO, and a comprehensive search across multiple databases without language restrictions, ensuring a broad and unbiased inclusion of studies. The independent data extraction and risk of bias assessment by multiple authors enhance the review's reliability. The use of both random-effects and fixed-effect models effectively addresses heterogeneity. However, the review also has limitations. The small number of included studies limits the robustness of findings and prevents a reliable assessment of publication bias. Variability in study protocols and patient characteristics contributes to heterogeneity, potentially affecting the generalizability of results. Additionally, some included studies had unclear or high risk of bias in specific domains.
Recommendations for Further Research
Future research should focus on large-scale, multicenter RCTs to confirm the benefits of warm saline in diverse populations and settings. Studies should also explore optimal temperatures and other variables influencing pain and satisfaction, along with long-term outcomes to develop comprehensive, evidence-based guidelines for clinical practice.
Conclusion
Warm saline as a distension medium during office hysteroscopy significantly reduces procedural pain and enhances patient satisfaction. These findings support the adoption of warm saline to improve patient experience and compliance, promoting a more patient-centered approach in gynecological care.
References
- Ahmed ME, Hashad AM, El-Skaan RG, et al. Effect of warm fluid distension media in relieving pain in outpatient hysteroscopy: randomized controlled trial. HJOG. 2024;23(2):124-132.
- Abdallah KS, Gadalla MA, Breijer M, et al. Uterine distension media for outpatient hysteroscopy. Cochrane Database Syst Rev. 2021;11(11):CD006604.
- Cingiloglu P, Mooney S, McNamara H, et al. Pain experience with outpatient hysteroscopy: a prospective cohort study. Eur J Obstet Gynecol Reprod Biol. 2024;300:302-308.
- Sewell T, Fung Y, Al-Kufaishi A, et al. Does virtual reality technology reduce pain and anxiety during outpatient hysteroscopy? A randomised controlled trial. BJOG. 2023;130(12):1466-1472.
- Kalmegh S, Patvekar M. Does the temperature of distension medium affect pain perception in AH? J Clin Diagn Res. 2025;19(1):QC13-15.
- Kapur S, Gruber A, Sekar H, et al. Does temperature of distending medium matter in outpatient hysteroscopy? A double-blinded cohort control observational study of room temperature versus warmed saline. J Obstet Gynaecol Res. 2020;46(3):485-489.
- Gulucu S, Cakmak B. Warm distension fluid reduces pain severity in office hysteroscopy: a randomized controlled trial. Ann Saudi Med. 2021;41(3):135-140.
- Nair VG, Mahajan R, Aziz A, et al. Effectiveness of warm saline for pain relief in office hysteroscopy: a prospective randomized control trial. Int J Clin Obstet Gynaecol. 2020;4(4):85-88.
- Tawfek ME, Hemeda HM, Ibrahim MA. The effectiveness of warm saline distension media on relieving pain in outpatient office hysteroscopy: a randomized controlled clinical trial. J Gynecol Reprod Med 2019;3(1):1-7.
- Evangelista A, Oliveira MAP, Crispi CP, et al. Diagnostic hysteroscopy using liquid distention medium: comparison of pain with warmed saline solution vs room-temperature saline solution. J Minim Invasive Gynecol. 2011;18(1):104-107.
- Sharma S, Roy KK, Rai R, et al. Assessment of pain at different steps of diagnostic hysteroscopy using room temperature normal saline versus warmed normal saline solution as distension medium: a randomized controlled trial. Gynecol Minim Invasive Ther. 2022;11(1), 41-46.
- Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151(4):264.
- Green S, Higgins JPT, Alderson P, et al. Cochrane Handbook: Cochrane Reviews: Ch 8: Assessing risk of bias in included studies. Cochrane Handbook Syst Rev Interventions. 2011:3-10.
- Higgins JPT, Thompson SG, Deeks JJ, et al. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557-560.
- Egger M, Smith GD, Schneider M, et al. Bias in meta-analysis detected by a simple, graphical test. BMJ. 2015;14:1-16.
- Terrin N, Schmid CH, Lau J, et al. Adjusting for publication bias in the presence of heterogeneity. Stat Med. 2003;22:2113-2126.
- Craciunas L, Sajid MS, Howell R. Carbon dioxide versus normal saline as distension medium for diagnostic hysteroscopy: a systematic review and meta-analysis of randomized controlled trials. Fertil Steril. 2013;100(6):1709-14.e1-4.
- Baradwan S, Khalil M, Alshahrani MS, et al. Warm saline effectiveness for pain relief in office hysteroscopy: a systematic review and meta-analysis of randomized controlled trials. J Obstet Gynaecol Res. 2022;48(7):1523-1530.
- De Silva PM, Stevenson H, Smith PP, et al. A systematic review of the effect of type, pressure, and temperature of the distension medium on pain during office hysteroscopy. J Minim Invasive Gynecol. 2021;28(6):1148-59.e2.
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Author Info
Mohammed Abdelrazeq#, Salwa Neyazi1, Khalid Akkour1, Nada Alayed1, Omar Alzaydan1, Eman Al Shehri1, Shadan Binsaeedan1, Ahmed Sherif1,2*, Alhassan Khedr2, Sondos Al Hawamdeh3, Mohammed Alatawi4, Mohammad Atlam5,6, Munirah Mohammed Binmosa1 and Karim Abdelsalam72Department of Obstetrics and Gynecology, Faculty of Medicine, Ain Shams University, Cairo, Egypt
3Department of Obstetrics and Gynecology, Doctor Sulaiman Alhabib Medical Group, Riyadh, Saudi Arabia
4Department of Obstetrics and Gynecology, Faculty of Medicine, Tabuk University, Tabuk, Saudi Arabia
5Anesthesia Registrar, Department of Anesthesia, Saudi German Hospital, Makkah, Saudi Arabia
6PHD in Anesthesia and Intensive Care, El Azhar University, Cairo, Egypt
7Department of Obstetrics and Gynecology, Faculty of Medicine, Helwan University, Helwan, Egypt
#Equally contribution
Copyright:This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.