Original Article - (2021) Volume 16, Issue 3
Ultrasound monitoring of uterine involution in the postpartum period
Irina Arkadievna Ozerskaya*, Vladimir Alexandrovich Ivanov and Aleksandr Vladimirovich KovynevReceived: 17-Feb-2021 Published: 28-Sep-2021
Abstract
Aim: to assess the rate of uterine involution and cavity changes on 3-4-5th day after spontaneous labor and caesarean delivery.
Materials and methods: The ultrasound examination of the uterus was conducted over 558 women in the postpartum period. On the 3rd day after delivery, 177 women were examined, on the 4th day – 299, and on the 5th day – 82. Vaginal delivery occurred in 454 (81.4%) patients, and 104 (18,6%) had caesarean delivery. In all cases there were precipitous labors, with single alive fetus, weighting 2640-4870g. Transabdominal ultrasound examination was conducted by one physician. The uterine volume was calculated by following formula: А∙В∙С∙0,523, where A is the uterine corpus length (cm), B is the anteroposterior diameter (cm), С is the transverse diameter (cm), and 0,532 is the coefficient. Similarly, data of the volume of the uterine cavity was obtained, and endometrial echo complex was analysed. For estimation of the rate of uterine involution and cavity reduction, the ratio of the volume of the cavity to the volume of the uterine body was calculated with the formula: Vcavity: Vuterus ∙ 100%.
Results: The condition of the uterine cavity, which decreases in anteroposterior diameter and volume, has the most important value for the evaluation of the postpartum period. Outrunning contraction of uterine cavity compare to the myometrium demonstrates the ratio of cavity to uterine body volume, which decreases from 8.0 per cent by 3rd day to 4.7 per cent by 5th day. If a hematometra persists, there was no reliable increase in uterine volume. Compare to the norm, the cavity of the uterus is reliably (p<0.05) larger than endometrial echo complex anteroposterior diameter, in the volume and in the ratio of the cavity to the volume of the uterus. Presence of retained placental tissue on the 3-4th day of the puerperium does not lead to subinvolution of the uterus, and also, it has no effect to the endometrial echo complex anteroposterior diameter and the cavity volume (p<0.05). Сaesarean delivery with normal postoperative period, and the presence of a uterine leiomyoma with a diameter less 30 mm, do not increase the volume of the uterus, neither its cavity, if compare to the normal rates.
Conclusion: When assessing the course of the postpartum period for 3-5 days, the state and size of the cavity should be given more importance than the uterus; the uterine volume is subject to pronounced individual fluctuations.
Keywords
Diagnostic ultrasound; Postpartum period; Uterine volume; Endometrial echo complex anteroposterior diameter; Uterine cavity volume
Introduction
The final stage of the gestational process is the postpartum period, during which there is a reverse development of the uterus associated with finish of pregnancy. Postnatal uterine involution takes place within 1.5-2 months. During this time, the uterus, weighing approximately 1 kg the day before delivery, reduces to the standard 70-80 g [1]. Multiple factors are considered to influence the contracting function: age, parity of birth, gestosis, anaemia, fetal weight, birth anomalies, etc. [2-4], but other researchers do not prove this [1,5-7].
According to the unanimous opinion of many local and foreign authors, ultrasound examination is the main method of diagnosing puerperium disorders. It is proposed to measure the linear dimensions of the uterus and the anteroposterior diameter of the endometrial echo complex [2], uterine area [4], linear dimensions, uterine volume and cavity anteroposterior diameter [8,9], uterine volume, and endometrial echo complex anteroposterior diameter [7], or the length and transverse diameter of the uterus exceptionally, in conjunction with the median complex [10] or without it [1], and etc. One of the methods that were used for predicting sub-involution in the postnatal period is the measurement of uterine anteroposterior diameter and endometrial echo complex in 2 hours and on the 3rd day after delivery with calculation of the involution coefficient [11, 12]. In this regard, we should agree with the opinion of J. De Winter and his co-op. (2017) [13], that there is no standardization of postnatal ultrasound examination of the woman’s uterus in our country or abroad.
Nowadays, discharge from a maternity hospital after physiological delivery happens on the 3rd day [14], and after the caesarean section – on the 4-5th day [15]. Uterine ultrasound examination is recommended before discharge to ensure there are no complications in the postpartum period.
Research aims: to assess the rate of uterine involution and cavity changes on the 3-4-5th day after spontaneous labor and caesarean delivery.
Materials and Methods
From November 2012 to June 2013, an ultrasound examination of the uterus of 558 women during the postnatal period was carried out at the maternity department of the 72 Moscow City Hospitals. In the period from November 2012 to June 2013, an ultrasound examination of the uterus of 558 women during the postnatal period was conducted.
On the 3rd day after delivery, 177 (31.7%) women were examined, on 4th day - 299 (53.6%) and for 5th day – 82 (14.7%). The age of the patients ranged from 17 to 42 years (30 + 6.4 years).
454 (81.4%) patients had vaginal births and 104 (18.6%) had caesarean section. There were 293 (52.5%) primiparous women, 235 (42.1%) women who had birth for the second time, and 30 (5.4 %) multiparous women. In all cases, at term deliveries were ascertained, with one alive fetus weighing 2640-4870 grams (3472 + 518 grams).
Hematometra was recorded based on increased volume of uterine cavity, with heterogeneous internal contents, without Color Doppler signals (Fig. 1.). Subsequently, these women underwent evacuation of blood clots, which was the verification of the diagnosis. In cases where there was no intervention, and the patients were classified with a normally proceeding puerperium.
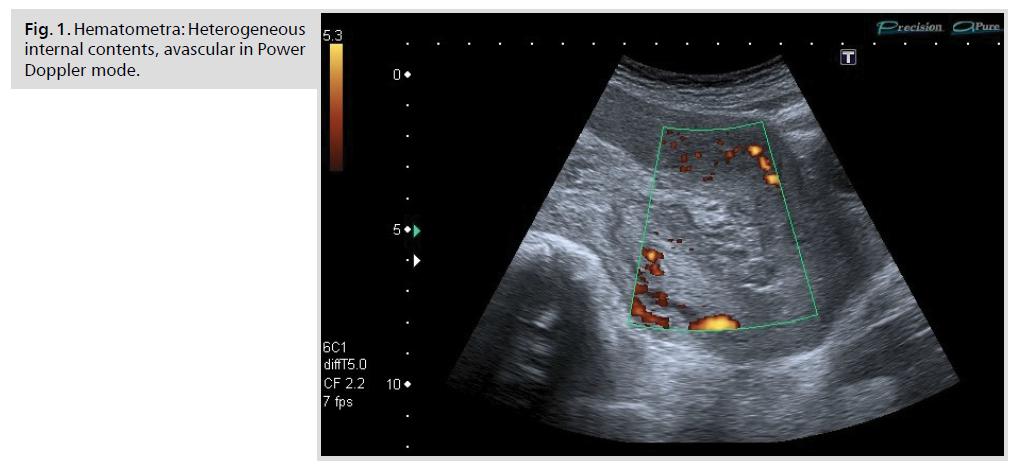
Figure 1: Hematometra: Heterogeneous internal contents, avascular in Power Doppler mode.
The diagnosis of retained placental tissue was based on the detection of parietal echogenic area with vessels therein and in the adjacent sub-endometrial zone with low-resistant and high velocity blood flow (Fig. 2.). Subsequent vacuum aspiration with histological examination of removed tissue under ultrasound control allowed placing these postpartum women into corresponding groups.
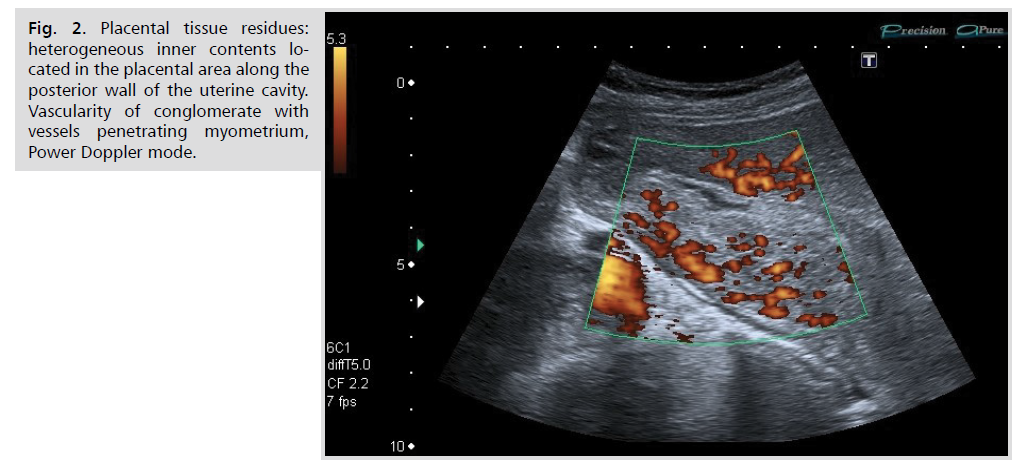
Figure 2: Placental tissue residues: heterogeneous inner contents located in the placental area along the posterior wall of the uterine cavity. Vascularity of conglomerate with vessels penetrating myometrium, Power Doppler mode.
The analysis did not include women with premature births, multiple pregnancies, and uterine anomalies. Considering that the large-sized leiomyoma delays the postpartum involution of the uterus [16], and small fibroids do not affect the reduction potential [6], the study did not include women with fibroids greater than 30 mm in diameter. In order to perform the correct analysis, women, who were after caesarean section or having a leiomyoma with hematometra, as well as retained placental tissue, have been excluded from the study.
Ultrasound study was performed by one specialist on two different apparatus: Aplio 500 (Toshiba, Japan) and IU22 (Philips, Netherlands) with convex multi-frequency transducers, frequency range 2-5 MHz. The transabdominal approach was used to measure the length and anteroposterior diameter of the uterus in the sagittal plane, while the transverse diameter was measured in transverse plane. Uterine volume was calculated according to the formula: А∙В∙С∙0,523, where A is the uterine corpus length (cm), B is the anteroposterior diameter (cm), С is the transverse diameter (cm), and 0.523 is the coefficient. Similarly, data on the volume of the uterine cavity was obtained (Fig. 3, 4.). To estimate the rate of uterine involution and cavity reduction, the ratio of the uterine cavity volume to the uterine body volume was calculated according to the formulae: Vcav: Vuter∙ 100%.
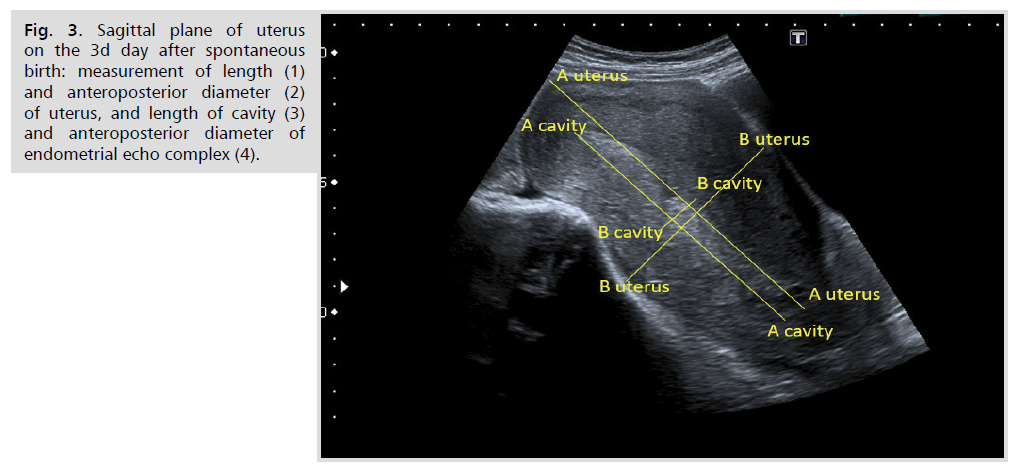
Figure 3: Sagittal plane of uterus on the 3d day after spontaneous birth: measurement of length (1) and anteroposterior diameter (2) of uterus, and length of cavity (3) and anteroposterior diameter of endometrial echo complex (4).
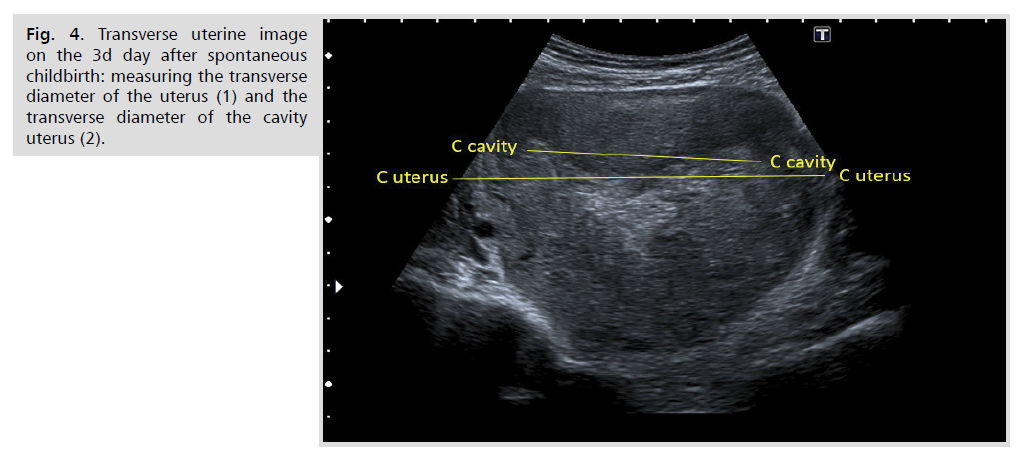
Figure 4: Transverse uterine image on the 3d day after spontaneous childbirth: measuring the transverse diameter of the uterus (1) and the transverse diameter of the cavity uterus (2).
The results were processed in standard statistical methods. Considering that part of the data was not subject to the normal distribution, all results are presented as median (50th percentile), 5-95th percentile and minimum – maximum. The median parity hypothesis was tested with the Mann-Whitney U-test. The differences were considered reliable at p<0.05. The relationship between the two variables was determined by Spearman correlation analysis. Coefficient values of 0.3 and less were assessed as weak relationship, values which were greater than 0.3 but less than 0.7 - medium relationship, and values of 0.7 and above were indicators of strong relationship.
Results
Among patients with spontaneous deliveries, linear sizes and volume of the uterus were gradually decreasing, with reliable (p<0.05) changes in the anteroposterior diameter and transverse diameter of the uterine body on the 4th day after the delivery compared to the 3rd day, and with transverse diameter changes on the 5th day compared to the 4th day.
The uterine cavity decreased in all dimensions. While the volume of the cavity and the ratio of the cavity to the volume of the uterus showed reliable (p<0.05) differences between the 3-4-5th days, the endometrial echo complex was almost the same on the 5th day after delivery compared to the 4th day (Tab. 1, 2).
| Days | Indicators | n | Length | Antero posterior diameter |
Transverse diameter | Volume |
|---|---|---|---|---|---|---|
| 3 | 127 | 125,5 100,8-150,0 81,5-172,8 |
76,8 56,3-91,3 48,3-101,0 |
122,8 95,5-144,8 91,0-156,0 |
599,2 334,5-831,0 290,8-1012,2 |
|
| 4 | 190 | 125,4 94,2-159,2 71,0-164,8 |
69,4 52,7-87,2 21,4-94,0 |
125,0 102,7-153,5 85,8-168,3 |
567,6 345,9-869,8 146,4-1043,5 |
|
| 5 | 35 | 119,9 101,1-141,1 90,0-156,0 |
69,0 54,0-86,6 51,0-107,8 |
130,3 110,0-145,2 94,0-148,0 |
547,3 365,8-736,8 283,2-934,4 |
|
| р, 3rd day | 0,57 | < 0,05 | < 0,05 | 0,17 | ||
| р, 4th day | 0,93 | 0,26 | 0,26 | 0,76 | ||
Tab. 1. The linear body sizes and volume of the uterus in the postnatal period after spontaneous timely birth.
| Days | Indicators | n | Endometrial echo complex | Vcav | Vcav/Vuter |
|---|---|---|---|---|---|
| 3 | 127 | 13,7 7,8-25,0 6,0-33,2 |
43,0 22,4-77,5 14,6-114,3 |
8,0 3,9-13,3 2,1-21,9 |
|
| 4 | 190 | 10,5 5,5-21,4 4,0-27,0 |
33,5 12,3-60,7 8,6-89,5 |
6,0 2,9-8,9 1,6-11,6 |
|
| 5 | 35 | 10,0 3,3-22,8 2,5-27,0 |
23,2 10,9-50,0 9,9-69,0 |
4,7 1,9-8,9 1,8-10,1 |
|
| р, 3th day | < 0,05 | < 0,05 | < 0,05 | ||
| р, 4th day | 0,39 | < 0,05 | < 0,05 | ||
Tab. 2. Endometrial echo complex, uterine cavity volume (Vcav) and cavity to uterine body volume ratio (Vcav/Vuter, %) in the postnatal period after spontaneous labors.
The involution of the uterus had a different nature after caesarean section. The volume of the uterus on the 4th day was almost the same as on the 3rd day. By the 5th day the uterus volume was smaller than in vaginal births, however no reliable differences were identified.
After caesarean section anteroposterior diameter of the endometrial echo complex and volume of uterine cavity were not different from those of women with spontaneous births. The ratio of the volume of the cavity to the volume of the uterus was reliably lower (р<0,05) on the 3rd day than in case of vaginal delivery (Tab. 3, 4).
| Days | Indicators | n | Length | Antero posterior diameter |
Transverse diameter | Volume |
|---|---|---|---|---|---|---|
| 3 | 23 | 122,0 109,3-151,9 107,0-164,0 |
71,5 62,9-80,6 62,0-81,0 |
130,5 99,8-154,9 93,0-163,0 |
611,7 432,0-924,2 395,7-1007,4 |
|
| 4 | 51 | 129,0 101,4-149,0 98,0-161,0 |
74,4 59,0-82,8 58,0-96,0 |
129,3 102,4-150,0 82,0-164,0 |
614,5 401,3-899,0 302,6-927,9 |
|
| 5 | 30 | 123,0 93,0-148,5 91,0-153,0 |
65,0 54,0-87,8 52,0-107,8 |
131,0 109,0-145,9 109,0-155,0 |
495,4 393,5-872,5 369,7-934,4 |
|
| р, norm for 3rd day | 0,99 | 0,21 | 0,33 | 0,81 | ||
| р, norm for 4th day | 0,51 | 0,17 | 0,58 | 0,20 | ||
| р, 3rd day C-section | 0,86 | 0,86 | 0,95 | 0,95 | ||
| р, norm 5th day | 0,81 | 0,69 | 0,84 | 0,98 | ||
| Р, 4th day C-section | 0,36 | 0,30 | 0,75 | 0,34 | ||
Tab. 3. Linear sizes and volume of uterus after Caesarean section.
| Days | Indicators | n | Endometrial echo complex | Vcav | Vcav/Vuter |
|---|---|---|---|---|---|
| 3 | 23 | 12,0 5,9-17,8 5,0-20,0 |
35,2 16,4-60,3 13,3-73,3 |
5,9 3,0-9,0 2,8-9,0 |
|
| 4 | 51 | 10,0 5,2-19,0 4,0-28,0 |
29,2 10,8-64,0 8,6-73,5 |
5,1 2,2-9,3 2,2-9,4 |
|
| 5 | 30 | 9,0 6,9-20,0 6,7-20,0 |
25,7 14,9-40,7 14,7-42,3 |
4,2 2,1-8,8 1,8-9,1 |
|
| р, norm for 3rd day | 0,95 | 0,09 | <0,05 | ||
| р, norm for 4th day | 0,57 | 0,93 | 0,38 | ||
| р, 3rd day C-section | 0,55 | 0,79 | 0,64 | ||
| p, norm 5th day | 0,71 | 0,78 | 0,72 | ||
| р, 4th day C-section | 0,89 | 0,07 | 0,67 | ||
Tab. 4. Endometrial echo complex, volume of uterine cavity (Vcav) and cavity to uterine body volume ratio (Vcav/Vuter, %) in post-caesarean period.
Small size leiomyoma, with a diameter less 30 mm, causes a slight increase in the volume of the puerperal uterus, however, it has not led to a reliable change in the figures compared to those of mothers with unchanged myometrium.
The endometrial echo complex and the uterine cavity volume after cesarean section did not differ significantly from those obtained in women with spontaneous labor. The ratio of the uterus cavity volume to the uterus body volume was reliably lower (p<0.05) than for women without a leiomyoma (Tab. 5, 6).
| Days | Indicators | n | Length | Antero posterior diameter | Transverse diameter | Volume |
|---|---|---|---|---|---|---|
| 3 | 6 | 126,0 122,4-126,9 122,0-127,0 |
70,0 67,3-84,4 67,0-86,0 |
128,0 116,3-140,6 115,0-142,0 |
634,2 572,1-654,6 565,1-656,9 |
|
| 4 | 23 | 130,0 115,0-153,0 113,0-160,0 |
70,0 51,5-91,0 44,0-93,0 |
134,0 115,0-158,0 110,0-163,0 |
622,7 489,6-1030,4 474,6-1190,7 |
|
| 5 | 8 | 132,5 102,6-149,7 100,0-150,0 |
74,5 54,0-87,4 52,0-88,0 |
142,5 121,1-166,5 119,0-169,0 |
722,5 382,5-969,3 323,6-988,3 |
|
| р, norm for 3rd day | 0,86 | 0,95 | 0,48 | 0,54 | ||
| р, norm for 4th day | 0,10 | 0,63 | 0,06 | 0,15 | ||
| p, 3rd day, myoma | 0,14 | 0,75 | 0,50 | 0,44 | ||
| р, norm 5th day | 0,51 | 0,79 | 0,27 | 0,35 | ||
| р, 4th day, myoma | 0,80 | 0,97 | 0,52 | 0,78 | ||
Tab. 5. The linear sizes and volume of the uterus with leiomyoma in the postpartum period.
| Days | Indicators | n | М-echo | Vcav | Vcav/Vuter |
|---|---|---|---|---|---|
| 3 | 6 | 14,0 10,4-17,6 10,0-18,0 |
39,8 31,0-41,2 30,0-41,4 |
6,3 5,4-6,3 5,3-6,3 |
|
| 4 | 23 | 11,0 7,0-19,0 5,0-20,0 |
37,3 21,4-85,2 16,1-117,8 |
6,1 3,5-9,2 3,1-9,9 |
|
| 5 | 8 | 16,0 10,3-20,0 10,0-20,0 |
52,0 36,9-80,0 34,8-84,4 |
8,2 5,6-11,6 5,6-11,8 |
|
| р, norm 3rd day | 0,84 | 0,96 | <0,05 | ||
| р, norm 4th day | 0,57 | 0,25 | 0,64 | ||
| р, 3rd, myoma | 0,56 | 0,45 | 0,63 | ||
| р, norm for 5th day | 0,15 | 0,07 | 0,12 | ||
| р, 4th day, myoma | 0,33 | 0,40 | 0,29 | ||
Tab. 6. Endometrial echo complex, uterine cavity volume (Vcav) and ratio of cavity volume to uterine body volume (Vcav/Vuter, %) with by leiomyoma in the postpartum period.
The presence of the hematometra did not affect the volume of the uterus, which had the same rate of involution as for the patients without postpartum complications. However, the transverse diameter of the uterus was reliably lower on the 3rd day (p<0.05) than a norm.
All dimensions of the uterine cavity were reliably higher (p<0.05) than those for healthy mothers. After the evacuation the hematometras and the endometrial echo complex, the volume of the cavity and the volume ratio of the uterus cavity to the uterus body remained reliably higher (p<0.05) than a norm, while on the 5th day all the parameters were almost the same as on the 4th day (Tab. 7, 8). Repeated evacuation of the uterine cavity content was performed on 6 (12.2%) patients.
| Days | Indicators | n | Length | Antero posterior diameter |
Transverse diameter | Volume |
|---|---|---|---|---|---|---|
| 3 | 14 | 123,0 100,6-169,2 100,1-172,8 |
73,2 59,4-81,1 53,4-81,8 |
113,1 98,3-125,8 95,6-129,0 |
559,3 386,6-663,1 321,2-663,9 |
|
| 4 | 26 | 118,0 100,2-149,0 95,0-150,0 |
70,0 60,0-96,2 44,0-106,0 |
125,0 98,0-144,0 89,0-149,0 |
550,3 355,4-722,0 241,8-792,5 |
|
| 5 | 9 | 104,5 87,7-130,0 81,0-131,0 |
79,5 55,5-90,6 52,0-92,0 |
122,5 100,5-132,7 98,0-133,0 |
498,0 331,6-740,9 323,6-754,2 |
|
| р, norm for 3rd day | 0,59 | 0,31 | <0,05 | 0,08 | ||
| р, norm for 4th day | 0,18 | 0,24 | 0,51 | 0,70 | ||
| р, 3rd day, hematometra | 0,36 | 0,75 | 0,51 | 0,43 | ||
| р, norm 5th day | 0,11 | 0,31 | 0,08 | 0,51 | ||
| р, 4th day, hematometra | <0,05 | 0,63 | 0,38 | 0,51 | ||
Tab. 7. Linear size and volume of the uterus with hematometra at the postnatal period.
| Days | Indicators | n | М-echo | Vcav | Vcav/Vuter |
|---|---|---|---|---|---|
| 3 | 14 | 21,0 15,0-31,6 14,4-33,2 |
59,8 41,0-112,0 33,4-114,3 |
14,4 10,1-21,7 9,6-21,9 |
|
| 4 | 26 | 18,0 10,2-26,6 10,0-28,0 |
57,9 43,6-97,5 33,3-102,8 |
10,9 8,3-16,5 8,1-18,1 |
|
| 5 | 9 | 20,5 11,8-25,6 10,0-27,0 |
49,9 34,5-85,1 34,4-85,5 |
11,0 8,4-13,7 8,2-13,9 |
|
| р, norm for 3rd day | <0,05 | <0,05 | <0,05 | ||
| р, norm for 4th day | <0,05 | <0,05 | <0,05 | ||
| р, 3rd day, hematometra | <0,05 | <0,05 | <0,05 | ||
| р, norm for 5th day | <0,05 | <0,05 | <0,05 | ||
| р, 4th day, hematometra | 0,48 | 0,41 | 0,49 | ||
Tab. 8. Endometrial echo complex, volume of uterine cavity (Vcav) and ratio of the volume of the cavity to the volume of the uterus body (Vcav/Vuter %) with hematometra in postpartum period.
Retained placental tissue was diagnosed on the 3-4th day after delivery, and then it was removed under ultrasound control. On the 5th day, patients with this pathology were not present.
When retained placental tissue was detected, the linear dimensions and volume of the uterus did not differ significantly from those of healthy women except for the transverse diameter when a reliable decrease was observed (p<0.05) on the 4th day.
The anteroposterior diameter of the endometrial echo complex, the volume of the cavity and the ratio of the volumes of the cavity/uterus were within the norm (Tab. 9, 10).
| Days | Indicators | n | Length | Antero posterior diameter |
Transverse diameter | Volume |
|---|---|---|---|---|---|---|
| 3 | 7 | 113,2 96,0-136,3 95,0-138,0 |
85,7 72,8-98,8 72,0-101,0 |
125,0 108,8-149,5 108,0-154,0 |
651,0 417,7-898,7 413,6-903,0 |
|
| 4 | 9 | 112,6 96,4-138,4 95,0-145,0 |
76,6 59,1-98,1 58,0-103,0 |
117,8 109,4-128,0 109,0-129,0 |
521,0 435,7-611,1 425,0-614,9 |
|
| р, norm 3rd day | 0,16 | 0,06 | 0,67 | 0,59 | ||
| р, norm 4th day | 0,10 | 0,22 | <0,05 | 0,09 | ||
| р, 3rd remains of placental tissue | 0,96 | 0,22 | 0,38 | 0,22 | ||
Tab. 9. Linear body sizes and volume of the uterus with the presence of retained placental tissue in the postpartum period.
| Days | Indicators | n | М-echo | Vcav | Vcav/Vuter |
|---|---|---|---|---|---|
| 3 | 7 | 17,0 12,8-20,0 12,0-20,0 |
53,9 22,3-66,3 19,8-66,3 |
7,4 5,2-8,6 4,6-8,7 |
|
| 4 | 9 | 14,0 9,7-22,6 9,0-25,0 |
38,5 18,8-49,9 18,3-52,6 |
6,9 4,2-9,3 4,0-9,4 |
|
| р, norm 3rd day | 0,14 | 0,82 | 0,31 | ||
| р, norm 4th day | 0,08 | 0,74 | 0,32 | ||
| р, 3rd remains of placental tissue | 0,45 | 0,21 | 0,57 | ||
Tab. 10. Endometrial echo complex, uterine cavity volume (Vcav) and ratio of cavity volume to uterine body volume (Vcav/Vuter, %) with retained placental tissue in postpartum period.
The correlation between the cavity volume and the volume of the uterine body was analysed. A moderate degree of correlation (r = 0.46) was identified among women with vaginal birth, after caesarean section (r = 0.38), and with a hematometra (r = 0.56), while the correlation degree was high in cases of uterine leiomyoma and residual placental tissue. The anteroposterior diameter of the endometrial echo complex and the volume of the cavity after cesarean section did not differ significantly from those obtained in women with spontaneous labor. (r = 0.72), and in the case of retained placental tissue (r = 0.88).
A low degree correlation (r < 0.30) between the rate of uterine regression and the age of women was determined, as well as parity of births, while the weight of the neonate had moderate effect (r = 0.35).
Discussion
Multiple factors influence the rate of regression of the uterus after delivery. Different factors were widely discussed in medical literature: the age problems of primiparas mothers, obstetric anamnesis, genital and extragenital pathology, pregnancy course, uterine overstretch (multiple births, polyhydramnios, large fetus), obstetric complications, intrauterine and operative vaginal delivery. In our own study a moderate correlation degree (r = 0.35) was found between the uterine involution and fetal weight, both low and heavy. Age and parity did not affect the sizes of the postnatal uterus. According to the results of V. Paliulite et al. (2017) [4], who examined primiparas and multiparous mothers after uncomplicated vaginal births on the 1st, 3rd, 10th, 30th, 42th, and 60th day of puerperium, noted that there was no reliable difference in uterine volume, but there was a tendency of slower involution in multiparous women.
The dimensions of the postpartum uterus have different rates of change in length, anteroposterior diameter, transverse diameter and volume. Thus, if the length decreased by 4.5%, from 3 days to 5 days, then the anteroposterior diameter - by 10.2%, and the transverse diameter increased by 6.1%, so the uterus has slight variation in length, but it expands and flattens. Since these processes are asynchronous, the volume of the uterine body at the 5th day is 91.3% of the volume by the 3rd day. In the most complete research article by L.F. Mozheiko and M.S. Verbitskaya [8] these patterns were not identified, while the numerical values of length and anteroposterior diameter in our papers are comparable, but the transverse diameter measured by our Belarusian colleagues is much less. A similar situation can be seen when comparing the results of the dissertation study by N.V. Ustyuzhanina [12], while in the article by N.N. Naumkin [2] all linear dimensions were significantly smaller. Probably due to the limited number of women analysed (31, 35 and 55 people among the compared researches), compare to 352 postpartum patients in our own study. In addition, the measurement method may be important, but it cannot be established in the specified articles. Difficulties in measuring length may arise in identifying the uterine internal os, due to on the 3-5th day after delivery the cervix is not formed yet, while the second point is the furthest point of the uterine fundus. The anteroposterior diameter (front to rear) and transverse diameter of the uterus should be measured at the level where the highest values are available. The only paper found that describes the measurement method is an article by I.A. Straznikov and L.I. Dyatlova [17]. Based on a survey of 71 women after uncomplicated spontaneous labor, T. Wataganara et al. (2015) [7] proved the presence of a strong correlation (r>0.7) between 2D ultrasound examination of the volume of the uterus and the 3D ultrasound.
In the analysis of uterine volume, there are marked individual variations when the indicators have multiple ranges. For example, on the 3rd day the minimum volume was 290.8 cc and the maximum volume was 1012.2 cc; on the 4th day - 146.4 cc and 1043.5 cc; on the 5th days - 283.2 cc and 934.4 cc respectively. The contraction of the uterus may be influenced by the specific anatomical and morphological structure of myometrium, such as the ratio of muscle cells to connective tissue, the degree of the layers expression, including the supravascular layer, which is characterized by the so-called median longitudinal muscle band [1]. It is extremely variable and formed due to the change in the direction of the muscle bundles along the uterine median line, continues in uterine ligaments and affects the birth activity [18].
The uterine cavity changes its shape in the postpartum period. Thus, if by the 3rd day the maximum endometrial echo complex expansion is more often observed closer to the bottom, then by 5th day - closer to the inner os. The decrease in the anteroposterior diameter of the endometrial echo complex was reliably significant with each subsequent day of the postnatal period and by the 4th day the anteroposterior its diameter was 10.5 (95 CI, 5.5-21.4) mm.
According to the measurement methodology adopted in our country and recommended by the consensus of the international experts of the IETA [19], the anteroposterior diameter of the endometrial echo complex should be measured at the widest point perpendicular to the wall of the uterus. Strict adherence to the methodology will make it possible to obtain correct measurements and compare the results of different authors.
In scientific publications great attention is paid to the state of the uterine cavity in women in puerperia. In a detailed review of 30 foreign publications by J. De Winter et al. (2017) [13] indicate that not so much the size and, accordingly, the volume of the uterus are important for assessing the course of the postpartum period, but the state of the cavity, including such parameters as the thickness (anteroposterior size) and volume of the cavity, as well as its contents. Most of the researchers in the mentioned survey believe that by the 3-4th day the anteroposterior diameter of a normal uterine cavity should be not more than 15 mm, with avascular cavity boundaries and heterogeneous internal content without color doppler signals.
Cavity volume decrease is faster than a decrease of myometrium. Thus, while the volume of the uterus was 94.7% of the 3rd day volume, the volume of the cavity was 77.9%. The ratio of the cavity volume to the uterine body volume shows that by the 3rd day the ratio is 8.0%, by the 4th day- 6.0% and by the 5th day - 4.7 %, therefore there is asynchronous contraction with cavity outstripping as compared to myometrium. T. Wataganara et al. (2015) also noted that uterus involution did not depend on a progressive thinning of the endometrial echo complex [7].
With hematometra, the anteroposterior diameter of the endometrial echo complex changes slightly: by the 3rd day - 21.0 (95 CI, 15.0-31.6) mm, by the 4th day - 18.0 (95 CI, 10.2-26.6) mm, by the 5th day - 20.5 (95 CI, 11.8-25.6) mm. The rate of decrease in the volume of the cavity was progressive, but not as pronounced as in healthy postpartum women, and the ratio of the volume of the cavity to the volume of the body of the uterus exceeded the norm by almost or more (on the 5th day) than 2 times.
In the case of retained placental tissue, the frequency of which is 1% [20], the sizes of the uterus and its cavity do not significantly differ from uncomplicated puerperium, which is fully consistent with the results of our own research. This is probably due to small pathological areas and timely measures to remove them. Detection of a local thickening of the median complex of more than 10 mm due to echogenic or heterogeneous mass with vessels with a sensitivity of 98.1% [21] corresponds to placental tissue. The higher the vascularity of the intracavitary area, the more likely this pathology [22]. However, the absence of vascularity does not exclude the remnants of placental tissue [23]. Color/power doppler mode allows differential diagnosis between the remnants of placental tissue and blood clots [24]. 3D reconstruction of the coronal plane of the uterine cavity is similar in informational value to 2D ultrasound [25].
Involution of the uterus after cesarean section with uncomplicated course is practically no different from vaginal delivery. The absence of a uterine volume decrease on the 4th day is most likely due to surgical trauma and myometrial edema. On the 5th day the uterine volume was less than after spontaneous births, which is probably related to the use of uterotonic drugs after the surgery. Dysplasia of connective tissue may affect the contraction capacity of myometrium and scar formation, leading to subinvolution and incompetent scar [26].
A careful hygiene of the uterus during surgery results in reliably lower ratio of cavity volume to uterine body volume by the 3rd day compare to the vaginal birth. A similar trend is noted by J.H. Kristoschek et al. (2017), who examined women on the 2nd day after caesarean section [9], and by A.M. Prijko et al. (2015) [5]. K.P. Fuller and D.M. Feldman (2015) [27] found that in the uncomplicated course of the postoperative period, the heterogeneous content in the uterine cavity is much less than in spontaneous delivery.
The presence of fibroids with a diameter of not more than 30 mm does not affect the rate of uterine involution. The cavity also does not have significant differences in the size of the endometrial echo complex, and in the volume, and in the ratio of the cavity volume to the volume of the uterine body. The same results on the analysis of the uterus and the state of its cavity were obtained in the work of G.N. Karimova et al. (2016) [6].
Conclusion
1. The most important factor for the assessment of the duration of the postpartum period is the condition of the uterine cavity, which decreases in anteroposterior diameter from 13.7 mm (95 CI, 5,5-21,4, p<0,05) on the 4th day, 10,0 mm (95 CI, 3,3-22,8) on the 5th day. The volume of the uterine cavity decreases from 43.0 cc (95 CI, 22.4-77.5) by the 3rd day, 33.5 cc (95 CI, 12.3-60.7, p<0.05) by the 4th days and 23.2 (95 CI, 10.9-50.0, p<0.05) by the 5th day.
2. The involution of the uterus occurs progressively, with large individual fluctuations. By the 3rd day the uterus volume is 599.2 cc (95 CI, 334.5-832.5), by the 4th day - 567.6 cc (95 CI, 345.9-869.8), by the 5th day - 547.3 cc (95 CI, 365.8-736.8).
3. The advance of the contraction of the uterine cavity in comparison with the myometrium is confirmed by a change in the ratio of the cavity volume to the volume of the uterine body, which decreases from 8.0% (95 CI, 3.9-13.3) on the 3rd day to 6.0% (95 CI, 2, 9-8.9, p <0.05) on day 4 and up to 4.7% (95 CI, 1.9-8.9, p <0.05) on day 5.
4. If the hematometra exists, there is no significant increase in the volume of the uterus. The cavity of the uterus is reliably (p<0.05) greater than the norm in terms of the anteroposterior diameter of the endometrial echo complex, the volume and the ratio of the volume of the cavity to the volume of the uterus body.
5. The detection of retained placental tissue on the 3-4th day of puerperia does not lead to subinvolution of the uterus, and also does not affect the anteroposterior diameter of the endometrial echo complex and the volume of the cavity (p<0.05).
6. The Caesarean section with uncomplicated postoperative course, as well as the presence of uterine fibroids with a diameter of less than 30 mm, do not lead to an increase in the volume of the uterus, including its cavity, in comparison with the norm.
Thus, when assessing the course of the postpartum period for 3-5 days, one should give greater importance to the state and size of the cavity than to the uterus, the volume of which is subject to pronounced individual fluctuations.
Authors Contributions
(A) Study Design · (B) Data Collection · (C) Statistical Analysis · (D) Data Interpretation · (E) Manuscript Preparation · (F) Literature Search · (G) Funds Collection
References
- Kolpakova EV. Predicting the rate of postpartum uterine involution. Author's abstract. MMSc. Tomsk, 2007. 24 p.
- Naumkin NN. Features of postpartum care in women giving birth with uterine subinvolution. AG-info. 2009; 4: 39-48.
- Morozova NI, Kwashenko VP, Babenko OM et al. Possibilities of prevention in women with uterine involution disorder. Med Social Prob Fam. 2014; 19 (1): 18-21.
- Paliulite V, Drasutiene GS, Ramamauskaite D et al. Physiological Uterine Involution in Primiparous and Multiparous Women: Ultrasound Study. Obstet Gynecol Int. 2017; 2017; 6739345. doi: 10.1155/2017/6739345
- Paridko AM, Baev OR, Lunkov SS et al. Echographic characteristics of the uterus in the early and remote period after abdominal birth. Obstet & Gynaecol. 2015; 10:41-46.
- Karimova GN, Shmakov RG, Yermina OV et al. Modern approaches to the echographic monitoring of the involution of the uterus in the postnatal period: influence on the tactics of the administration. Obstet & Gynaecol. 2016; 3: 43-49.
- Wataganara T, Phithakwatchara N, Komoltri C et al. Functional three-dimensional sonographic study of the postpartum uterus. J Matern Fetal Neonatal Med. 2015; 28 (18): 2221-2227.
- Mozheiko LF, Verbytskaya MS. Sonographic examination of the uterus and uterine blood flow in the diagnosis of postpartum endometritis. Medical panorama. 2011; 6: 8-12.
- Kristoschek JH, de Sá Moreira RA, Silva FCD, Vellarde GC. Ultrasonographic Evaluation of Uterine Involution in the Early Puerperium. Rev Bras Ginecol Obstet. 2017; 39 (4): 149-154.
- Sokol ER, Casele H, Haney EI. Ultrasound examination of the postpartum uterus: what is normal? J Matern Fetal Neonatal Med. 2004; 15 (2): 95-99.
- Mulic-Lutvica A, Bekuretsion M, Bakos O, Axelsson O. Ultasonic evaluation of the uterus and uterine cavity after normal vaginal delivery. Ultrasound Obstet Gynecol. 2001; 18 (5): 491-498.
- Ustyuzhanina NV Prediction and prevention of postpartum septicaemia complications in the conditions of the perinatal center. MMSc. Science Institute. Perm, 2013. p 24.
- De Winter J, De Raedemaecker H, Myes J, Jacquemyn Y. The value of postpartum ultrasound for the diagnosis of retained product of conception: A systematic review. Fact Views Vis. Obgyn. 2017; 9: 207-216.
- Order of the Ministry of Health of Russia dated 01.11.2012 No. 572n On approval of the Procedure for the provision of medical care in the field of obstetrics and gynecology (except for the use of assisted reproductive technologies). Material from the Reference System "Chief Physician" https://vip.1glv.ru/#/document/99/902379345/ZAP2OF43P7/?of=copy-caaf202304
- Federal clinical guidelines "Management of postpartum women after abdominal delivery". M., 2013. p. 21.
- Fominova GV, Lyalichkina NV, Kosenko YuYu et al. The course of the gestational process and delivery of patients with uterine myoma. Modern problems of science and education. 2018; 4: 138-145.
- Strazhnikov IA, Dyatlova LI. Ultrasound criteria for uterine involution after cesarean section. Basic research. 2008; 11: 54-55.
- Kokh LI, Bissé TV. A method for predicting the course of an act of labor. Patent No. 98104796/14 dated 1999 http://www.ntpo.com/patents_medicine/medicine_1/medicine_423.shtml
- Leone FP, Timmerman D, Bourne T et al. Terms, definitions and measurements to describe the sonographic features of the endometrium and intrauterine lesions: a consensus opinion from the International Endometrial Tumor Analysis (IETA) group. Ultrasound Obstet Gynecol. 2010; 35 (1): 103–112.
- Weissbach T, Haikin-Herzberger E, Bacci-Hugger K et al. Immediate postpartum ultrasound evaluation for suspected retained placental tissue in patients undergoing manual removal of placenta. Eur J Obstet Gynecol Reprod Biol. 2015; 192: 37-40.
- Matijevic R, Knezevic M, Grgic O, Zlodi-Hrsak L. Diagnostic accuracy of sonographic and clinical parameters in the prediction of retained products of conception. J Ultrasound Med. 2009; 28: 295-299.
- Sellmyer MA, Desser TS, Maturen KE. et al. Physiologic, histologic, and imaging features of retained products of conception. Radiographics. 2013; 33 (3): 781-796.
- Steinkeler J, Coldwell BJ, Warner MA. Ultrasound of the postpartum uterus. Ultrasound Q. 2012; 28: 97-103.
- Smorgick N, Krakov A, Maymon R et al. Postpartum Retained Products of Conception: A Novel Approach to Follow-Up and Early Diagnosis. Ultraschall Med. 2017; 21.
- Belachew J, Axelsson O, Eurenius K, Mulic-Lutvica A. Three-dimensional ultrasound does not improve diagnosis of retained placental tissue compared to two-dimensional ultrasound. Acta Obstet Gynecol Scand. 2015; 94 (1): 112-116.
- Shchukina NA, Bujanova SN, Chechneva MA et al. The reasons for the formation of untenable scar on the uterus after the caesarean section, and the role of the dislocation of the connective tissue. Russian Gazette of Obstetrician-Gynecologist. 2018; 5: 4-11.
- Fuller KP, Feldman DM. To establish normal ultrasonographic findings for the postpartum uterus. J Reprod Med. 2015; 60 (1-2): 3-5.
Author Info
Irina Arkadievna Ozerskaya*, Vladimir Alexandrovich Ivanov and Aleksandr Vladimirovich KovynevCopyright:This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.