Research - (2023) Volume 18, Issue 2
Transversus abdominis block; direct visualization vs. ultrasound guided for post-operative cesarean section pain
Mohamed A. Ali*, Khaled H. Swedan, Mohamed S. Sweed, Hanan M. Ali and Rania H. MostafaReceived: 10-Aug-2022, Manuscript No. gpmp-22-71883; Editor assigned: 11-Aug-2022, Pre QC No. P-71883; Reviewed: 20-Oct-2022, QC No. Q-71883; Revised: 20-Mar-2023, Manuscript No. R-71883; Published: 30-Jun-2023
Abstract
Background: The transverse abdominis plane (TAP) block provides effective analgesia after lower abdominal surgeries including cesarean section (CS). TAP block can be performed under ultrasound guidance (US-TAP) or under direct visualization (DV-TAP).
Aim: To compare analgesia-efficacy between US-TAP vs. DV-TAP
Patients and methods: Forty women who attended Ain Shams University Maternity Hospital for elective CS were randomly divided into 2 groups; DV-TAP (n=20) and US-TAP (n=20).
Results: Both groups showed a similar analgesics-use during first postoperative 24 and 48 hours. DV-TAP showed lower pain score than US-TAP; it was significant; immediately, postoperative 6 and 24 hours, and non-significant postoperative 12 hours. Incidence of complications were the same between the two.
Conclusion: DV-TAP was more effective than US-TAP in cases of post-CS-analgesia. Postoperative using of analgesics, complications did not differ between the two.
Keywords
Transversus abdominis block; Direct visualization; Ultrasound guided; Cesarean section
Introduction
Following operations including caesarean sections, cholecystectomy, prostatectomy, hysterectomy, and transplant surgery, nerve root or myofascial irritation at the abdomen wall is a typical cause of pain. A risk factor for postpartum depression and ongoing pain includes severe acute pain following a caesarean surgery [1].
To avoid a variety of unfavorable side effects like respiratory issues, venous thromboembolism, and an extended hospital stay, post-operative analgesia is crucial. The pain management needs to be both effective and safe for the nursing infant [2].
The two main types of pain experienced during caesarean sections are somatic (caused by the abdominal wall incision) and visceral (from the uterus). A variety of abdominal surgeries, including abdominal wall reconstruction, have adopted the standard of care of adequately controlling post-operative pain while reducing the administration of opioids [3].
Since they are effective against both components, systemic or neuraxial opioids are the mainstay of postoperative pain management. However, side effects like vomiting, nausea, and respiratory depressions are frequently linked to opiate use [4].
Non steroid anti-inflammatory drugs alone may be insufficient to treat post cesarean pain. Currently, multimodal analgesic technique involving abdominal nerve block with parenteral analgesics is becoming popular for these patients. The transversus abdominis plane (TAP) block has been used for post-operative pain relief in various abdominal surgeries as part of the multimodal analgesic approach. It creates satisfactory somatic analgesia with insignificant or no visceral blockade [5].
Transverse abdominis plane (TAP) block anesthetize the trunks of iliohypogastric and ilioinguinal nerves. TAP is a neurovascular plane located between the internal oblique and transverse abdominis muscles and nerves supplying abdominal wall pass through this plane before supplying anterior abdominal wall. In abdominal surgeries, TAP blocks have been shown to reduce overall narcotic use and narcotic associated side effects, improve overall pain, and reduce hospital length of stay [6].
TAP blocks can be carried out by an anesthesiologist using either a "blind" technique that relies on anatomical landmarks and the sensation of a blunt needle "popping" through the myofascial planes, or an ultrasound guided technique that makes use of real-time sonography to see the correctly positioned needle tip. A rising number of studies show that TAP blocks performed by surgeons, which involve directly observing the entry of a needle into the proper plane and the bulging of the transversus abdominis muscle as fluid enters the proper plane, are both secure and efficient [7].
Patients and Methods
This study was conducted on forty hemodynamic stable pregnant women, who attended for elective cesarean sections. They were randomized into 2 equal groups; group (I): included 20 women who underwent direct visualization TAP block (DV-TAP) and group (II): included 20 women who underwent ultrasound guided TAP block (US-TAP).
Study type: The study type was double armed interventional trial.
Study place: The study was conducted at Ain Shams University Maternity Hospital.
Study period: The study was conducted from April to June 2022.
Inclusion criteria
1. Hemodynamic stable pregnant women.
2. Maternal age: 20-40 years old.
3. BMI: 20-30 kg/m2.
Exclusion criteria
1. Contraindication to regional anesthesia as coagulopathy.
2. Infection at the side of injection.
3. Allergy to study medications.
4. Patients not able to understand numeric rating scale (NRS).
Sampling method
A convenience sample
Sample size
40 pregnant women (20 cases in each group)
Sample size justification
Using the STATA tool, the sample size was computed using a 5 percent alpha error and a 90 percent power setting. Result from previous study [8] showed that the mean post-operative pain at Day 0 was 2.35 ± 2 in DV-TAP compared to 4.12 ± 1 in US-TAP. Based on this, 20 cases per group were needed.
Allocation and randomization
Patients undergoing TAP block will be randomized using a computer-generated sequence 1:1 open or ultrasound guided TAP group.
Allocation and concealment
Each of the 40 women included in the study will be given a number from 1 to 40. The numbers will be put in 5 closed envelopes where each envelope will contain 8 numbers and each participant will pick a number from one of the envelopes. Through a computer based randomization, each number corresponded to a procedure either group 1 or 2.
Study procedures
Written informed consent was given by each woman for the surgical procedure and TAP blocks.
Transverses Abdominis Plane (TAP) block
All pregnant women received spinal anesthesia by anesthesia team according to the height of the women. All procedures were done by supervisors. The transverses abdominis plane (TAP) block was done by competent surgeon and competent anesthesiologist.
Group I: 20 women were subjected to direct visualization TAP blocks (DV-TAP) which was performed by a surgical team member following closure of the uterus and before closure of parietal peritoneum by using sharp needle which blunted by surgical team member.
TAP block was identified using 1 pop sensation. This pop indicated penetration of the fascia of transverses abdominis muscle. After calculation of toxic dose, 20ml bupivacaine (0.25%) were injected at each side from inside after aspiration into the intramuscular plane with a blunt needle under direct visualization. Confirmation of the correct plane of injection was made by observing the accumulation of injected bupivacaine causing the transverses abdominis muscle belly to bulge posteriorly (Fig. 1.).
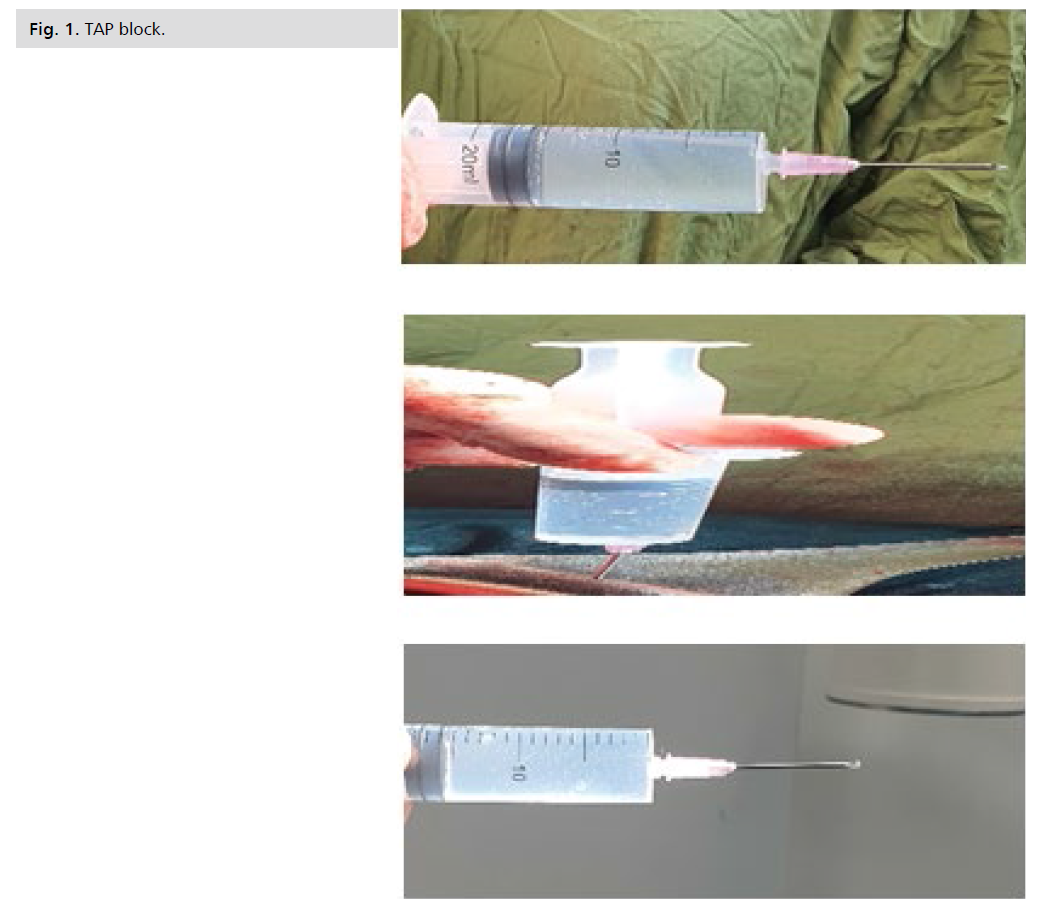
Fig 1. TAP block.
Group II: 20 women were subjected to ultrasound guided TAP blocks (US-TAP) which was performed immediately after the closure of the skin under the guidance of a trained attending anesthesiologist.
The mid-axillary line between the costal border and the iliac crest was chosen as the location for the ultrasound probe to be transverse to the abdomen. After determining the toxic dose, a 22 gauge echogenic needle was used under real-time ultrasound guidance to inject 20 ml of 0.25 percent bupivacaine into the inter-muscular plane between the internal oblique and the transverses abdominis muscle on each side after aspiration. Before administering bupivacaine, the correct intramuscular plane was expanded by the buildup of a test flush, which was visible as the needle point was localized within the correct plane.
In this study, we measured outcomes compared to previous STATA and STATA calculations as numeric rating scale (NRS) that was done every 6 hours in the first 12 hours and once in the next 12 hours, where zero time was started after the spinal anesthesia was resolved and the women started to move their legs, rescue analgesia time (time for 1st request for analgesics) if NSR was more than 3, they received pain killer as non-steroidal anti-inflammatory drugs within 48 hours, analgesic consumption, incidence of complications of TAP as skin hematoma, transient femoral nerve palsy, amount of analgesics at home with frequency and late visual analogue scale at home and wound infection.
Results
Age in Group (I) was ranged between 22-37 years with mean ± S.D. 29.00 ± 4.81 years while in Group (II) was ranged between 20-40 years with mean ± S.D. 30.50 ± 6.00 years. There was no statistically significant differences between groups where P=0.42 (Tab. 1.).
| Variables | Group | t* | P value | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Group I (DV-TAP) (N=20) |
Group II (US-TAP) (N=20) |
|||||||||
| Min. | Max. | Mean | SD | Min. | Max. | Mean | SD | |||
| Age (years) | 22.00 | 37.00 | 29.10 | 4.81 | 20.00 | 40.00 | 30.50 | 6.00 | 0.81 | 0.42 NS |
Tab. 1. Comparison between two groups as regard to patient’s age (years).
Weight in Group (I) was ranged between 68.0-90.0 kg with mean ± S.D. 76.25 ± 5.87 kg while in Group (II) was ranged between 69.0-92.0 kg with mean ± S.D. 79.18 ± 6.47 kg. There was no statistically significant differences between groups where P=0.14. Height in Group (I) was ranged between 155-175 cm with mean ± S.D. 163.75 ± 5.41 cm while in Group (II) was ranged between 157-177 cm with mean ± S.D. 167.05 ± 6.01 cm. There was no statistically significant differences between groups where P=0.08. BMI in Group (I) was ranged between 25.91-29.67 kg/m2 with mean ± S.D. 28.40 ± 0.93 kg/m2 while in Group (II) was ranged between 25.97-29.67 kg/m2 with mean ± S.D. 28.34 ± 1.18 kg/m2. There was no statistically significant differences between groups where P=0.86 (Tab. 2.).
| Variables | Group | t* | P value | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Group I (DV-TAP) (N=20) |
Group II (US-TAP) (N=20) |
|||||||||
| Min. | Max. | Mean | SD | Min. | Max. | Mean | SD | |||
| Weight (Kg) | 68.00 | 90.00 | 76.25 | 5.87 | 69.00 | 92.00 | 79.18 | 6.47 | 1.50 | 0.14 NS |
| Height (cm) | 155.00 | 175.00 | 163.75 | 5.41 | 157.00 | 177.00 | 167.05 | 6.01 | 1.83 | 0.08 NS |
| BMI (Kg/m2) | 25.91 | 29.67 | 28.40 | .93 | 25.97 | 29.67 | 28.34 | 1.18 | 0.18 | 0.86 NS |
Tab. 2. Comparison between two groups as regard to patient’s measurements.
Gravidity in Group (I) and Group (II) was ranged between 1-6. There was no statistically significant differences between groups where P=0.75. Parity in Group (I) and Group (II) was ranged between 0-5. There was no statistically significant differences between groups where P=0.98. History of abortion in Group (I) show that 5(25.0%) had history of abortion while in Group (II) 4(20.0) had history of abortion. There was no statistically significant differences between groups where P=1.00. History of previous CS in Group (I) show that 19(95.0%) had history of previous CS while in Group (II) 19(95.0%) had history of previous CS. There were no statistically significant differences between groups where P=1.00. History of medical history in Group (I) show that 3(15.0%) had a medical history while in Group (II) 6 (30.0) had a medical history. There was no statistically significant differences between groups where P=0.45. History of surgical history in Group (I) show that 4(20.0%) had a surgical history while in Group (II) 10(50.0%) had a surgical history. There were statistically significant differences between groups where P=0.05 (Tab. 3.).
| Variables | Group | X2* | P value | ||||
|---|---|---|---|---|---|---|---|
| Group I (DV-TAP) (N=20) | Group II (US-TAP) (N=20) | ||||||
| N | % | N | % | ||||
| Gravidity | 1.00 | 0 | 0.0% | 1 | 5.0% | 3.24 (FE) |
0.75 NS |
| 2.00 | 7 | 35.0% | 8 | 40.0% | |||
| 3.00 | 3 | 15.0% | 3 | 15.0% | |||
| 4.00 | 5 | 25.0% | 2 | 10.0% | |||
| 5.00 | 3 | 15.0% | 2 | 10.0% | |||
| 6.00 | 2 | 10.0% | 4 | 20.0% | |||
| Gravidity | 1-3 | 10 | 50.0% | 12 | 60.0% | 0.40 | 0.53 NS |
| >=4 | 10 | 50.0% | 8 | 40.0% | |||
| Parity | 0.00 | 1 | 5.0% | 1 | 5.0% | 1.40 FE |
0.98 NS |
| 1.00 | 7 | 35.0% | 8 | 40.0% | |||
| 2.00 | 5 | 25.0% | 3 | 15.0% | |||
| 3.00 | 4 | 20.0% | 4 | 20.0% | |||
| 4.00 | 2 | 10.0% | 3 | 15.0% | |||
| 5.00 | 1 | 5.0% | 1 | 5.0% | |||
| Parity | 0.00 | 1 | 5.0% | 1 | 5.0% | 0.39 FE |
1.00 NS |
| 1-2 | 12 | 60.0% | 11 | 55.0% | |||
| >=3 | 7 | 35.0% | 8 | 40.0% | |||
| Miscarriage | Yes | 5 | 25.0% | 4 | 20.0% | 0.14 FE |
1.00 NS |
| No | 15 | 75.0% | 16 | 80.0% | |||
| Previous CS | Yes | 19 | 95.0% | 19 | 95.0% | 0.00 FE |
1.00 NS |
| No | 1 | 5.0% | 1 | 5.0% | |||
| Medically | Yes | 3 | 15.0% | 6 | 30.0% | 1.29 FE |
0.45 NS |
| No | 17 | 85.0% | 14 | 70.0% | |||
| Surgically | Yes | 4 | 20.0% | 10 | 50.0% | 3.96 | 0.05 S |
| No | 16 | 80.0% | 10 | 50.0% | |||
Tab. 3. Comparison between two groups regarding patient’s obstetric history.
Using analgesic in Group (I) show that 20(100.0%) had to use it during first 24hr and 20(100.0%) had to use it in home during 48hrs after surgery while in Group (II) 20(100.0%) had to use it during first 24hr and 17(100.0%) had to use it in home during 48hrs after surgery. There were no statistically significant differences between groups (Tab. 4.).
| Variables | Group | X2* | P value | ||||
|---|---|---|---|---|---|---|---|
| Group I (DV-TAP) (N=20) |
Group II (US-TAP) (N=20) |
||||||
| N | % | N | % | ||||
| Analgesic use during first 24 hrs | Yes | 20 | 100.0% | 20 | 100.0% | - | - |
| No | 0 | 0.0% | 0 | 0.0% | |||
| Analgesic use in home during 48 hrs after surgery | Yes | 20 | 100.0% | 17 | 100.0% | - | - |
| No | 0 | 0.0% | 0 | 0.0% | |||
Tab. 4. Comparison between two groups as regard to patient’s using analgesic.
Numeric rating scale (NRS) in Group (I) after the spinal anesthesia had a mean ± S.D. 2.06 ± 1.06 and it was increased to be after 24 hours 3.72 ± 0.46 while in Group (II) after the spinal anesthesia had a mean ± S.D. 3.56 ± 1.20 and it was increased to be after 24 hours 4.11 ± 0.47. There were highly statistically significant differences between groups when comparing NRS after the spinal anesthesia, after 6 hours and after 24hours (Tab. 5. and Fig. 2.).
| Variables | Group | t* | P value | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Group I (DV-TAP) (N=20) |
Group II (US-TAP) (N=20) |
|||||||||
| Min. | Max. | Mean | SD | Min. | Max. | Mean | SD | |||
| Pain score 0 | 1.00 | 4.00 | 2.06 | 1.06 | 2.00 | 5.00 | 3.56 | 1.20 | 3.98 | <0.001 HS |
| Pain score 6 | 1.00 | 5.00 | 2.61 | 0.98 | 3.00 | 5.00 | 3.67 | 0.84 | 3.47 | 0.001 HS |
| Pain score 12 | 3.00 | 5.00 | 4.00 | 0.69 | 3.00 | 6.00 | 4.39 | 0.85 | 1.51 | 0.14 NS |
| Pain score 24 | 3.00 | 4.00 | 3.72 | 0.46 | 3.00 | 5.00 | 4.11 | 0.47 | 2.50 | 0.02 S |
Tab. 5. Comparison between two groups as regard to patient’s Numeric Rating Scale (NRS).

Fig 2. Numeric rating scale.
Complications in Group (I) show 19(95.0%) had no complications, 18(90.0%) had no Wound infection while in Group (II) 19(95.0%) had no complications, 15(88.2%) had no Wound infection. There were no statistically significant differences between groups (Tab. 6., Fig. 3. and Fig. 4.).
| Variables | Group | X2* | P value | ||||
|---|---|---|---|---|---|---|---|
| Group I (DV-TAP) (N=20) |
Group II (US-TAP) (N=20) |
||||||
| N | % | N | % | ||||
| Wound infection | Yes | 2 | 10.0% | 2 | 11.8% | 0.03 FE |
1.00 NS |
| No | 18 | 90.0% | 15 | 88.2% | |||
| Complications | Yes | 1 | 5.0% | 1 | 5.0% | 0.00 FE |
1.00 NS |
| No | 19 | 95.0% | 19 | 95.0% | |||
Tab. 6. Post-operative complications.
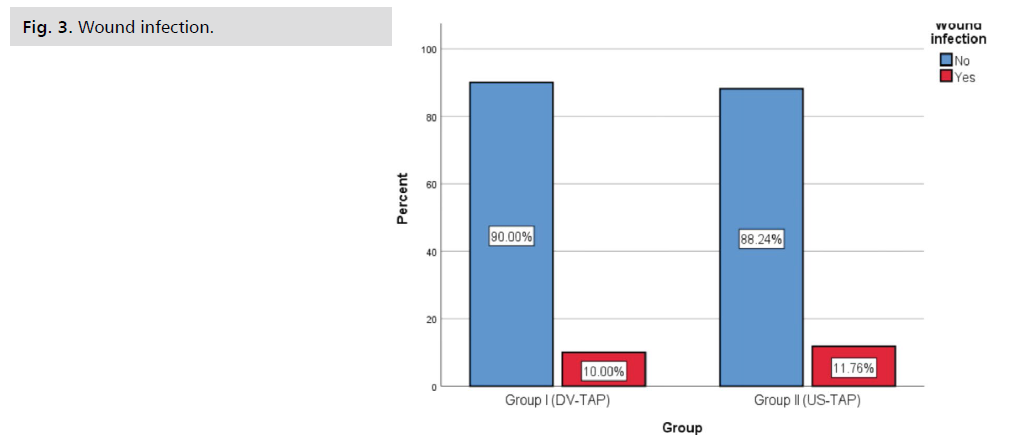
Fig 3. Wound infection.
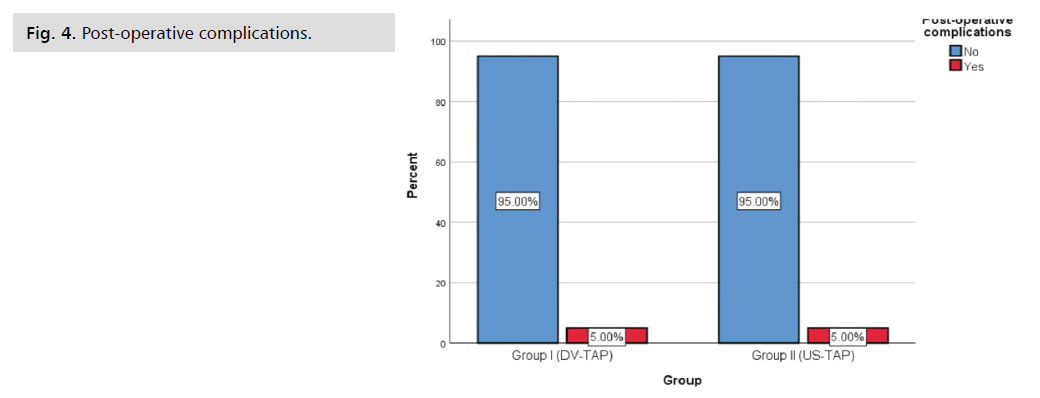
Fig 4. Post-operative complications.
Discussion
To our knowledge, there was only one published data that directly assess the efficacy of TAP block in patients undergoing cesarean section comparing between ultrasound guidance (US-TAP) and under direct visualization (DV-TAP).
Another study evaluated transversus abdominis plane blocks performed after open posterior component separation hernia surgeries using direct visualization vs. ultrasound guidance.
Regarding basal demographic data; statistical analysis of current results showed that there was no significant difference between both groups regarding age, weight, height, BMI, gravidity, parity, history of abortion, history of previous CS and medical disorders with p=0.42, 0.14, 0.08, 0.86, 0.75, 0.98, 1.00, 1.00 and 0.45 respectively. On the other hand, history of surgical operations were statistically significant higher in group II that might be have an impact on post-operative pain score of this group p=0.05.
The current study supported Urfalolu and colleagues' findings that BMI and mean age did not significantly differ between research groups, with p=0.154 and 0.490, respectively. They investigated the applicability, effectiveness, and outcomes of surgical transversus abdominis plane and ultrasound-guided transversus abdominis plane blocks in obese pregnant women who underwent caesarean sections while under general anaesthesia. A total of 75 pregnant women with a BMI of 30 or more were randomly assigned to either the surgical TAP block (ST group; n=37) or the ultrasound-guided transversus abdominis plane block (UT group; n=38) [9].
Doble and his colleagues agreed with current study and stated that the demographics of the patients were the same (including age, body mass index, comorbid conditions, American Society of Anesthesiologists [ASA] classification). They proposed that after open ventral hernia surgery, DV-TAP and US-TAP would both offer comparable postoperative analgesia. A retrospective analysis of 39 patients receiving TAP blocks with 266 mg of liposomal bupivacaine during open VHR with posterior component separation (PCS) was done [8].
Regarding postoperative analgesics; statistical analysis of current results showed that there was no significant difference between both groups regarding using of analgesics during first 24 and 48 hours after surgery with p> 0.05.
In agreement with current study, no significant differences in mean time to first analgesic requirement or total analgesic intake over 24 hours were reported across groups, according to Urfalolu and his colleagues (p=0.168 and p=0.539, respectively). Although there was no significant difference in median patient satisfaction scores across groups (p=0.962), our study did not look at women's satisfaction [9].
Against us and according to Doble and his colleagues, On postoperative days (POD) 0, 1, and 4, a substantial decrease in the amount of narcotics utilized was seen in the DV-TAP group as compared to the US-TAP group, but not on POD 2, 3, or >4. The average daily narcotic doses in the DV-TAP group were lower (80.7 vs. 167.7 mg; p=0.02), as well as the total amount of narcotics consumed while in the hospital (408.5 vs. 860.9 mg; p=0.013) [8].
Regarding patient’s numeric rating scale (NRS); statistical analysis of current results showed that pain score was lower in group I (DV-TAP) than group II (US-TAP) immediately, 6 hours and 24 postoperatively p=<0.001, 0.001 and 0.02 respectively, however no statistical difference was noted between both groups 12 hours postoperatively p=0.14.
In comparison to the current study, Urfalolu and his colleagues noted that no significant variations in visual analogue scale scores were identified across the groups at any time, which could be attributed to differences in BMI of the study population, sample size, and pain assessment scale utilised [9].
Doble and his colleagues agreed with current study and stated that the immediate postoperative time appears to be when DV-TAP blocks offer greater analgesia. Patients in the US-TAP group required significantly greater narcotic medication during their hospital stay in order to obtain comparable post-operative pain scores [8].
Regarding postoperative complications; statistical analysis of current results showed that there was no significant difference between both groups regarding wound infection and other complications p=1.00 and 1.00 respectively.
Nausea was noted in four patients in each of the UT and ST groups, according to Urfalolu and his colleagues; one patient in the UT group had itching, which was explained by a drop in opiate consumption after both surgeries in that patient. No P-values could be calculated because these data were unsuitable for statistical analysis [9].
The current investigation supported Doble and his colleagues' claims that there were no TAP block-related issues in the post-operative period or the first 30 days after the treatment [8].
Last but not least, the current investigation refuted the claims made by McDermott and colleagues that using the conventional landmark-based approach to the TAP blocks results in imprecise needle and local anesthetic insertion and an overly high incidence of peritoneal placement. In order to evaluate the placement of the needle tip and local anesthetic during TAP blocks using the landmark-based "double-pop" technique utilizing ultrasound, they designed a prospective, blinded trial in an adult general surgery population. After putting 36 adult patients under general anesthesia, a TAP block was administered bilaterally using the traditional landmark-based method. Then, utilizing ultrasonography, the needle location and local anesthetic distribution were documented. When administering the block, the anesthetist was not shown the ultrasound images. The experiment enrolled 36 adult patients but was terminated early due to an extremely high number of peritoneal needle insertions. Only 17 (23.6%) of the injections had the local anesthetic and needle tip disperse in the proper plane. Subcutaneous tissue 1 (1.38%), external oblique muscle 1 (1.38%), plane between external and internal oblique muscles 5 (6.94%), internal oblique muscle 26 (36.1%), transversus abdominis muscle 9 (12.5%), and peritoneum 13 in the remainder 55 (76.4%) were all the areas where the needle was inserted (18 percent) [10].
Strengths
The current study's advantages stem from the fact that it was the first to evaluate the effectiveness of TAP block in caesarean section patients by contrasting ultrasound guidance (US-TAP) and under direct visualization (DV-TAP). All follow-up data were verified to be accurate, and only complete information was used in the data analysis. The same team performed all clinical assessments, caesarean sections, TAP blocks, and evaluations of research results.
Limitations
The COVID 19 pandemic, drug side effects, and some uncommon outcomes, such as injection site wound infection, necessitated a comparatively higher sample number, which led to the study's limitations. After blockade, the degree of sensorial block was not established, and only post-operative NRS was evaluated as part of the evaluation of the success of the blockade. However, due to patients receiving spinal anesthesia being unlikely to give accurate information about sensorial block during the early post-operative period and at later times, particularly in the T7-L1 dermatome region where blockade was provided and was enclosed in plaster, this evaluation could not be completed. A control group without a block was absent. Here, our main goal was to contrast the effectiveness and drawbacks of TAP blocks performed under direct visualization (DV-TAP) and ultrasound guidance (US-TAP). Due to a paucity of suitable pregnant women who completed the study criteria, we did not include a third control group.
Conclusion
Direct visualization TAP block (DV-TAP) was more effective than ultrasound guided procedure in cases of post cesarean section analgesic approach immediately and 6 hours postoperatively, however there were no differences between both methods reading postoperative using of analgesics, wound infection and other complications.
Statistical Analysis
With the aid of the IBM SPSS software package version 20.0, data were fed into the computer and evaluated (IBM Corp, Armonk, NY). Number and percentage were used to describe qualitative data. The normality of the distribution was examined using the Kolmogorov-Smirnov test. Utilizing range (minimum and maximum), mean, and standard deviation, quantitative data were described. The significance of the results was assessed at the 5% level.
Acknowledgment
Authors would like to thanks to Ain Shams University and the patients recruited in the study.
Funding
No funding sources
Conflict of Interest
None declared.
Ethical Approval
The study was approved by the Institutional Ethics Committee.
Authors Contribution
(A) Study Design · (B) Data Collection · (C) Statistical Analysis · (D) Data Interpretation · (E) Manuscript Preparation · (F) Literature Search · (G) No Fund Collection
References
- Montero AA, Carnerero CS, Vidal PI, et al. CDC guidelines for prescribing opioids for chronic pain. Semergen. 2017;43(4):e53-e54.
- Doble JA, Winder JS, Witte SR, et al. Direct visualization transversus abdominis plane blocks offer superior pain control compared to ultrasound guided blocks following open posterior component separation hernia repairs. Hernia. 2018;22:627-635.
- Fayezizadeh M, Majumder A, Neupane R, et al. Efficacy of transversus abdominis plane block with liposomal bupivacaine during open abdominal wall reconstruction. Am J Surg. 2016;212(3):399-405.
- Kerai S, Saxena KN, Taneja B. Post-caesarean analgesia: What is new?. Indian J Anaesth. 2017;61(3):200.
- McDermott G, Korba E, Mata U, et al. Should we stop doing blind transversus abdominis plane blocks?. Br J Anaesth. 2012;108(3):499-502.
- Nair A. Bilateral quadratus lumborum block for post-caesarean analgesia. Indian J Anaesth. 2017;61(4):362-3.
- Park JS, Choi GS, Kwak KH, et al. Effect of local wound infiltration and transversus abdominis plane block on morphine use after laparoscopic colectomy: A nonrandomized, single-blind prospective study. J Surg Res. 2015;195(1):61-66.
- Urfalıoğlu A, Bakacak M, Boran ÖF, et al. Ultrasound-guided vs. surgical transversus abdominis plane block in obese patients following cesarean section: A prospective randomised study. Rev Bras Anestesiol. 2017;67:480-486.
- Weibel S, Neubert K, Jelting Y, et al. Incidence and severity of chronic pain after caesarean section. Eur J Anaesthesiol. 2016;33(11):853-865.
- Young MJ, Gorlin AW, Modest VE, et al. Clinical implications of the transversus abdominis plane block in adults. Anesthesiol Res Pract. 2012;2012.
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Author Info
Mohamed A. Ali*, Khaled H. Swedan, Mohamed S. Sweed, Hanan M. Ali and Rania H. MostafaCopyright:This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.