Research - (2025) Volume 20, Issue 3
The rate of abnormal pap smear results in Iraqi women at Aldiwaniyah city
Shaimaa Abdulamer Nasir*Received: 20-Jun-2025, Manuscript No. gpmp-25-164835; Editor assigned: 23-Jun-2025, Pre QC No. P-164835; Reviewed: 15-Jul-2025, QC No. Q-164835; Revised: 23-Jul-2025, Manuscript No. R-164835; Published: 30-Sep-2025
Abstract
Background: In Iraq, there were 2.1 instances of cervical cancer for every 100,000 females of all ages, rendering to the World Health Organization (WHO). On top of that, 10.21 million Iraqi women aged 15 to 44 were at risk of getting cancer. Method: A cross-sectional training was directed at The Maternity and Paediatric Teaching Hospital in Aldiwaniyah city over a ten-month period, from February 15 to November 15, 2024. All 150 female patients who visited the cervical cancer screening unit throughout the study dated were comprised. In the cytology lab, smears were obtained with the Ayre's spatula, and the results were assessed using the system of Bethesda Scoring. use the Chi square test to highlight connections of demographic information and cytological results. For the significant variables, binary logistic regression was employed. A significance level of 0.05 was deemed to be present in our statistical study. Findings: The pap smear results for the majority of the sample (89.5%) were normal. Abnormal pap smear results were reported by 10.5% of the remaining women. The most common patient concerns were vaginal discharge (49.33%), irregular bleeding (20.66%), and after coital bleeding (2.6%). Only three incidences of cervical cancer were discovered. A statistically significant association was found in females under 45 and abnormal pap smears (p = 0.037 for both). While females who are 45 years old have increased the likelihood of having abnormal pap smears [OR=4.012; CI 96%], smoking increased the hazards [p=0.003; OR=0.021; CI 93%]. Conclusion: Smoking was significantly related to abnormal pap smear results in females under 45, and abnormal pap smears were found in 10.5% of the samples. It is necessary to initiate, advertise, and raise awareness of a cervical cancer screening program and the risk factors it involves.
Introduction
Cervical cancer results from aberrant cell proliferation in the cervical epithelium. Around 70% of cervical cancer cases are squamous cell carcinoma, with adenocarcinoma following in second. Cervicovaginal carcinoma causes over 7% of all female cancer deaths worldwide [1]. 85 percent of cervical malignancy cases appear in developed nations with insufficient screening strategies [2]. Cervical cancer is the second most mutual kind of malignancy in both men and women, after only lung cancer and breast cancer. According to estimates for 2018, Iraq discovers 244 new instances of cervical cancer each year. Cervical cancer kills 159 individuals every year. More than 99% of cervix cancers are caused by the sexually transmitted human papillomavirus (HPV) infection of high-risk types, which is intimately related to Cervical Intraepithelial Neoplasias (CINs), also known as precancerous lesions of the cervix, and cervical carcinomas [3]. Seventy percent of cervical tumors are types 16 or 18. Human Papillomavirus (HPV), smoking, low socioeconomic level, early marriage before the age of 18, first sexual contact at a early age, having several sexual relationships with her or her husband, and having multiple pregnancies all augment the danger of cervical cancer. Several variables increase the hazard of cervical cancer. It has been established that HPV is the leading cause of cervical cancer. The most common HPV genotypes associated with invasive cervical cancer are 16, 18, 31, 33, and 45. Normal cells divide faster as humans age. Normal cells divide faster in the first several years of life, allowing for growth. When a individual scopes adulthood, the common of cells division to substitute those that have died. Cancer occurs when the body's cancer-causing cells proliferate uncontrollably [4]. The cervix joins the vagina to the uterine body. The endocervix is the portion of the cervix adjoining the uterine body. The ectocervix is the portion of the cervix nearest to the vagina. Cervical malignancy develops at the squamocolumnar junction, which is made up of cells that line the cervix. The majority of the cells that cover the mucosa of the cervix are squamous and glandular. These two cell types come together in the transformative zone. The transformative zone shifts following pregnancy and delivery, as well as with a woman's age. The transformative zone is where cervical cancer usually starts [5]. The two most significant acts the woman can do to avoid cervical malignancy are to obtain the HPV vaccination and to get frequent screenings mentioned by the American Cancer Society (ACS) strategies. These guidelines are part of the American Cancer Society's Recommendations for the Prevention and Early Detection of Cervical Cancer, Version 6. Cervical malignancy is preventable thanks to the lengthy preinvasive period. Screening enables early detection and treatment [6]. Cytological screening for precancerous lesions and cervix cancer, as well as subsequent treatments for these lesions, have decreased the occurrence and fatality rate as of cervical cancer. The primary care level conducts a gynecologic examination as well as a Pap smear screening test to identify irregularities that could lead to cervical cancer. It is non-invasive, simple to use, and cheaply priced. When combined with routine screening and follow-up, the pap test can reduce the mortality risk from cervical malignancy by up to 80% [7]. The goal of this training was to investigate the association between anomalous pap smear findings and sociodemographic variables, as well as to explain the ratio of anomalous pap smear findings in a group of Iraqi women.
Methods
This cross-sectional study was carried out at Aldiwaniyah Maternity and Paediatric Teaching Hospital over a ten-month period, from February 15 to November 15, 2024. The sample consisted of female patients who visited the cervical cancer screening unit. Every patient who was missing to continuation was omitted as of the study; all sick were included for the whole term. Thus, the sample consisted of 150 instances in total. The Maternity and Paediatric Teaching Hospital granted ethical approval for the investigation. Patients' age, employment position, parity, marital status, use of hormonal contraceptives, smoking history, primary illness, and family history of maliganancy were all obtained by phone calls.
Following examinations, the results of speculum tests on individuals were recorded. The pap smear findings displayed that there was no specific inflammatory response, benign cellular abnormalities, including infections, epithelial cell lesions, comprising Atypical Glandular cells of Undetermined Significance (AGUS), and Atypical Squamous Cells of Undetermined Significance (ASC-US) and different grades of squamous intraepithelial lesions (SIL). All pap smear samples were sent to a cytological lab. Ayre's spatula was used to gather all cytological smears, which were then spread out on slides and examined in the cytology lab [7]. The Bethesda Scoring System was used to record the cytological diagnosis. The chi square assessment was used to highlight the relations among sociodemographic characteristics and anomalous and normal pap smear outcomes. For the significant variables, logistic regression was performed using a binary model. In completely statistical investigates, a P value of 0.05 was deliberated significant.
Results
With ages ranging from 20 to 58, the sample under investigation had an average age of (43.20+8.4). Tab. 1. displays the attributes of the examined sample. Most were married, nonsmokers, and housewives. 88 out of 150 individuals, or 57.4% of the sample, did not use combination oral contraceptives.
| Frequency (Percentage) | ||
|---|---|---|
| Age group | Less than 45 | 65(39.2%) |
| 45 and more | 85(60.8%) | |
| Parity | Nulliparous | 15(9.3%) |
| Primiparous | 78(52.6%) | |
| Multiparous | 57(38.1%) | |
| Age of marriage | Less than 20 | 92(68.1%) |
| More than 20 | 58(31.9%) | |
| Combined oral contraceptive pills | Yes | 62(42.6%) |
| No | 88(57.4%) | |
| occupation | Housewife | 112(74.66%) |
| Employed | 38(25.34%) | |
| Family history of cancer | Yes | 47(31.33%) |
| No | 103(68.67%) | |
| Smocker | Yes | 14(9.3%) |
| No | 136(90.7%) |
Tab. 1. Distributions of the demographic attributes and results of the sample (n=150).
The most frequent symptoms from patients were vaginal discharge (49.33%), irregular bleeding (20.66%), post-coital bleeding (2.6%), and after sex (3%) (Tab. 2., Tab. 3. and Fig. 1.).
| Patient complain | Frequency (Percentage) |
|---|---|
| Pain | 10(6.66%) |
| Abnormal vaginal bleeding | 14(9.3%) |
| Mixed post coital bleeding and others | 4(2.6%) |
| Irregular bleeding | 31 (20.66%) |
| Post-menopausal bleeding | 14(9.3%) |
| Vaginal discharge | 74(49.33%) |
| Asymptomatic | 3(2%) |
Tab. 2. Patient distributions by primary complaint (n=150).
| Pap smear result | Percentage | Frequency | |
|---|---|---|---|
| Abnormal | HSIL | 3.33% | 5 |
| LSIL | 3.33% | 5 | |
| Squamous cell carcinoma | 2.60% | 4 | |
| AGC-NOS | 3.33% | 5 | |
| Normal | inflammation | 36.00% | 54 |
| ASCUS | 27.33% | 41 | |
| NILM | 24.00% | 36 | |
| Total | 100% | 150 | |
Tab. 3. Detailed pap smear findings for the sample under study (n=150).
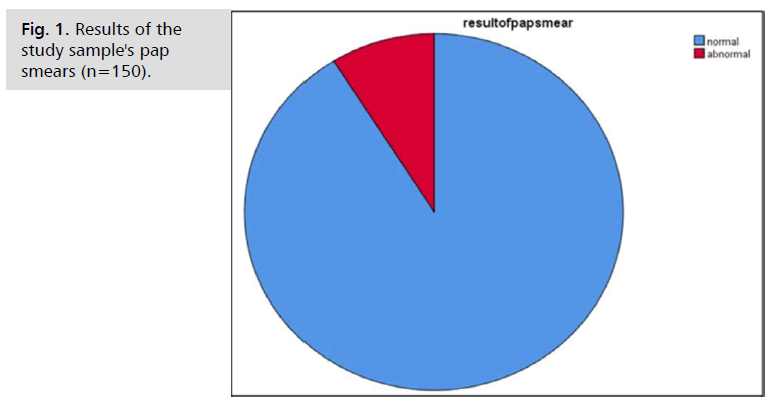
Fig. 1. Results of the study sample's pap smears (n=150).
However, no significant correlation was found between the patient's reported occupation as indicated in Tab. 4. and abnormal pap smear results. These factors included being 45 years of age or older, smoking, being multiparous, being married below the 20 years old, using combined oral contraception, and having a positive family history.
| Result of pap smear | ||||
|---|---|---|---|---|
| Abnormal | normal | P Value | ||
| Age group | Less than 45 | 18(12%) | 47(31.33%) | 0.037 |
| 45 and more | 26(17.33%) | 59(39.33%) | ||
| Parity | Nulliparous | 0 | 15(9.3%) | 0.00 |
| Primiparous | 0 | 78(52.6%) | ||
| Multiparous | 17(11.33%) | 40(26.66%) | ||
| Age of marriage | Less than 20 | 12(8%) | 80(53.33%) | 0.007 |
| More than 20 | 16(10.66%) | 24(28%) | ||
| Combined oral contraceptive pills | Yes | 7(4.66%) | 55(36.66%) | 0.031 |
| No | 14(9.33%) | 74(49.33%) | ||
| occupation | Housewife | 20(13.33%) | 92(61.33%) | 0.143 |
| Employed | 6(4%) | 32(21.3%) | ||
| Patient complain | Pain | 2(1.33%) | 8(5.33%) | 0.182 |
| Abnormal vaginal bleeding | 5(3.33%) | 9(6%) | ||
| Mixed post coital bleeding and others | 0 | 4(2.6%) | ||
| Irregular bleeding | 9(6%) | 22(14.66%) | ||
| Post-menopausal bleeding | 3(2%) | 11(7.33%) | ||
| Vaginal discharge | 10(6.66%) | 64(42.66%) | ||
| Asymptomatic | 0 | 3(2%) | ||
| Family history of cancer | Yes | 14(9.33%) | 33(22%) | 0.00 |
| No | 23(15.33%) | 80(53.33%) | ||
| Smocker | Yes | 9(6%) | 5(3.33%) | 0.00 |
| No | 24(16%) | 112((74.66%) | ||
Tab. 4. The study sample's distribution according to pap smear results and demographic traits.
Those who were 45 years old or more had a six-fold higher likelihood of having an abnormal pap smear [OR=4.012; CI 96%], according to binary logistic regression analysis for the variables (Tab. 5.).
| Odd ratio | 95% Confidence interval | ||
|---|---|---|---|
| Lower limit | Upper limit | ||
| Age of marriage | 0.097 | 0.011 | 0.847 |
| Age group | 3.045 | 0.722 | 58.036 |
| Occupation | 0.241 | 0.061 | 1.864 |
| Combined oral contraceptive pills | 0.176 | 0.022 | 0.977 |
| Smoker | 0.023 | 0.001 | 0.092 |
Tab. 5. Results of the accompanying factors for abnormal pap smear results in the investigation sample using binary logistic regression.
Discussion
About half of the samples tested in a 2014 Baghdad study had abnormal pap smear results, according to the study of Abdulla KN, et al. [7] and Abdulraheem AF, et al. [8]. In 2019, researchers found that 23.3% of the women surveyed had abnormal intraepithelial lesions. Presently, 10.5% of female samples from Iraq have abnormal pap smear results. Possible explanations for this disparity include differences in screening program competency and number of the patients. while, 3.8% was the reported figure in Jordan in 2017, and 4.9% in Saudi Arabia in 2011 [9,10]. Late presentation and lack of awareness could be contributing factors to the higher rate of abnormal pap smears in Iraq, where a cervical cancer screening platform is not yet in place. This study's 36.2% abnormal pap smear rate was similar to those of three previous Baghdad investigations in 2014 (ASCUS 10%, 11.2%, 10.1%, and 1.5%, respectively) and 2019 (11.2%, 10.1%, and 1.5%, respectively). This was lower than the prevalence rates in 2011 LSIL 0.09%, (ASCUS 2.99%, HSIL 0.68% in Saudi Arabia) and 2017 (ASCUS 2.90%, HSIL 0.68%, LSIL 5.09%, in India) [7,8]. [5,9] HSIL (0.48%). Consistent with previous research from Saudi Arabia (0.3%) and Baghdad (0.4%), only three patients (2%) were detected with cervical malignancy at the study period. Cultural and religious norms, as well as sexual practices, contribute to a low cervical cancer prevalence. Sexual relations between a man and a woman before they are married are forbidden by Islamic law in Iraq. Nonetheless, additional practices—such as the common practice of male circumcision in our country—also contribute. A statistically important increase in the risk of abnormal pap smear discoveries was observed for females aged 45 and above, in agreement with a 2019 study from Iraq (Baghdad) that indicated the average ages of patients with ASCUS (43.37 ± 0.8), HISL (44.91 ± 2.95), and LISL (38.91 ± 2.95) to be 40.5, 10.8, and 38.8 years, respectively. Furthermore, although a study in India in 2018 found that most of abnormal pap smear findings occurred in individuals aged 40 to 60, a study in Kirkuk in 2012 found that the average age of these findings was 47 years old. Binary logistic regression studies have shown a robust association between advanced age and aberrant pap smear findings [5,7,11,12]. This study confirms what Guarisi R, et al. [13] found that smoking increases the likelihood of getting an abnormal pap smear. In a 1999 study done in the US, et al. found a robust relation among smoking and cervical cancer [14]. In a 2009 study done in Argentina and Brazil, smoking was strongly associated with negative pap smear results even when the colposcopy came back negative. This conclusion, however, contradicts data from Saudi Arabia in 2018 [15], which failed to detect any correlation between smoking and abnormal pap smear findings. A statistical analysis also revealed a correlation among abnormal pap smear findings and factors like parity, age of marriage, using of combined hormonal contraceptives, and a family history of malignancy. Cervical abnormalities and premalignant alterations were linked to high parity, hormonal contraceptive use, and the main complaint (postcoital bleeding or vaginal discharge) in a 2016 Baghdad study [16]. Research in Saudi Arabia in 2018 [15] and Baghdad in 2020 [17] could not find a correlation between these traits and the cervix, despite the apparent relationship.
Conclusion
Approximately 10.5% of pap smears had abnormalities. Abnormal pap smear results were significantly associated with being a woman over 45, smoking, having more than one child, getting married below the age of 20 years, using combination oral contraception, and having a positive family history. These results highlight the necessity of developing a thorough cervical screening program, raising public knowledge of the condition and its risk factors, implementing preventative strategies, and making sure that individuals with abnormal pap smear results receive ongoing care.
References
- Hull R, Mbele M, Makhafola T, et al. Cervical cancer in low and middle‑income countries. Oncol Lett. 2020;20:2058-2074.
- Brahmana IB, Widiyatmoko A. Screening for pregnancy program patients with vaginal swab and pap smear Examination. Jurnal Aisyah: Jurnal Ilmu Kesehatan. 2022;7:489-494.
- Sogukpınar N, Saydam BK, Can HO, et al. Assessment of cervical cancer risk in women between 15 and 49 years of age: case of Izmir. Asian Pac J Cancer Prev. 2013;14:2119-2125.
- Hasan MY, Al Hashimi BA, Al Niyazee AA, et al. Prevalence of abnormal Pap smears among sample of Iraqi women attending Al Elweiya Cervical Screening Unit in Baghdad. J Cardiovasc Dis Res. 2020;11:120-124.
- Kashyap N, Krishnan N, Kaur S, et al. Risk factors of cervical cancer: a case-control study. Asia Pac J Oncol Nurs. 2019;6:308-314.
- Aggarwal P. Cervical cancer: can it be prevented?. World J Clin Oncol. 2014;5:775.
- Abdulla KN, Alheshimi SJ, Aljebory HS, et al. Evaluation of Pap smear data in Baghdad province. Int J Sci Res Pub. 2016;6:634-639.
- Abdulraheem AF, Khudhairi JM. Papanicolaou Smear Outcome of Referred Women to Health Facilities in Baghdad. Mustansiriya Med J. 2014;13:33-37.
- Balaha MH, Al Moghannum MS, Al Ghowinem N, et al. Cytological pattern of cervical Papanicolaou smear in eastern region of Saudi Arabia. J Cytol. 2011;28:173-177.
- Maraqa B, Lataifeh I, Otay L, et al. Prevalence of abnormal pap smears: a descriptive study from a cancer center in a low-prevalence community. Asian Pac J Cancer Prev. 2017;18:3117.
- Mohammed M, Mohammed K. Prevalence of abnormal cervical smears among females in Kirkuk governorate. Journal of Kirkuk university-scientific studies. 2012;7.
- Akinfolarin AC, Olusegun AK, Omoladun O, et al. Age and pattern of Pap smear abnormalities: Implications for cervical cancer control in a developing country. J Cytol. 2017;34:208-211.
- Guarisi R, Sarian LO, Hammes LS, et al. Smoking worsens the prognosis of mild abnormalities in cervical cytology. Acta Obstet Gynecol Scand. 2009;88:514-520.
- Scholes D, McBride C, Grothaus L, et al. The association between cigarette smoking and low-grade cervical abnormalities in reproductive-age women. Cancer Causes & Control. 1999;10:339-344.
- Shalabi MM, Ismael RI, ur Rahman S, et al. Prevalence and Risk Factors of Cervical Neoplastic Lesions in Patients Attending a Healthcare Specialty Clinic, King Abdulaziz Medical City, Saudi Arabia. J Cancer Ther. 2018;9:307-313.
- American cancer society. Cancer of cervix Causes, Risk Factors, and Prevention. cancer.org 2017.
- Hasan MY, Al Hashimi BA, Al Niyazee AA, et al. Prevalence of abnormal Pap smears among sample of Iraqi women attending Al Elweiya Cervical Screening Unit in Baghdad. J Cardiovasc Dis Res. 2020;11:120-124.
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Author Info
Shaimaa Abdulamer Nasir*Copyright:This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.