Research - (2022) Volume 0, Issue 0
The incidence of unplanned curettage in expectant versus medical and surgical management of spontaneous first trimester abortion
Eithar Mohammed*, Tarek Tamara, Sherif Ashoush and Gihan El-HawwaryReceived: 17-Jul-2022, Manuscript No. gpmp-22-69380; Editor assigned: 18-Jul-2022, Pre QC No. P-69380; Reviewed: 28-Jul-2022, QC No. Q-69380; Revised: 10-Aug-2022, Manuscript No. R-69380; Published: 29-Sep-2022
Abstract
Objective: The aim of our study was to compare and assess the incidence of unplanned uterine curettage between expectant management versus medical and surgical management within of first trimester missed and incomplete miscarriage. Patients and Methods: This Randomized controlled trial included 150 patients diagnosed with early fetal demise at less than 13 weeks’ gestation. They were recruited and assessed for eligibility from Ain Shams University Maternity Hospital. Cases were randomized according to a computer-generated random sequence into three groups; Expectant (A), Surgical (B) and Medical groups (C). the three groups were studied in regard to the incidence of hospital re-admission, gynaecological infection, the duration of clinical symptoms (pain, additional analgesia, vaginal bleeding), complications (fall in haemoglobin at 10-14 days, blood transfusion, unplanned consultations or admissions within 14 days and within eight weeks) and Efficacy.
Results: Our results indicated statistically significant difference (P<0.05) between studied groups as regard vaginal bleeding as a symptom of miscarriage. Regarding the post-intervention bleeding duration per days among the studied groups, our results indicated that bleeding duration was highly significant and the longest among the expectant group followed by the medical then the surgery groups (P<0.001). Our results indicated the presence of statistically significant difference (p-value<0.05) between studied groups as regard failed treatment and shift to surgery that was more prevalent in the expectant group followed by the medical group. Our results indicated no statistical significant difference between studied groups (expectant, medical and surgical groups) as regard emergency unplanned D&C due to heavy bleeding (p-value > 0.05).
Conclusion: The incidence of failed treatment and shift to surgery after expectant, medical and surgical management of spontaneous first trimester miscarriage was more prevalent in the expectant group followed by the medical group then the surgical group. Regarding complications, our results indicated a highly statistical significant difference between studied groups as regard hypotension. It was more prevalent in medical group followed by the expectant group then the surgical group.
Keywords
Low-lying placenta Unplanned Curettage; Expectant treatment; Medical and Surgical Management; Spontaneous First Trimester Abortion
Introduction
Spontaneous miscarriage complicates between 10% and 20% of pregnancies, and it is estimated that around 25% of all women will experience at least one miscarriage during their reproductive lives [1,2]. Miscarriage was usually treated by surgical curettage aiming for manual removal of any retained tissue therefore avoid the risk of infection and haemorrhage, the benefits of surgical management include appropriate timing for the patient and high success rates, however, surgical management has complications including Asherman’s syndrome caused by endometrial damage [2-4].
There are two alternative options to surgical management; expectant management and medical management that can be followed after diagnosing first trimester miscarriage. Expectant management allows spontaneous passage of the retained products of conception therefore, it is considered as a more natural option, while medical management includes medical evacuation of the uterus using synthetic prostaglandin analogues, or a combination of mifepristone or methotrexate with misoprostol [5].
Management of spontaneous first trimester pregnancy loss is usually determined by medical opinion and patient preference however, uncertainty exists about the preferred option in a given situation and there is a lack of clarity about the most meaningful outcomes, particularly from a woman’s perspective [6].
Post-miscarriage complications of the three methods of management occur as a result of several causes including infection, incomplete evacuation of the products of conception that lead to hemorrhagic complication, and injury from the surgical procedure itself [7].
Unplanned curettage intervention is applied in cases where there are retained products of placenta following the primary intervention to stop bleeding, eliminate infection or prevent long-term complications. Studies indicated significantly more unplanned admissions and unplanned surgical curettage occurred after expectant management in comparison with surgical or medical managements [8,9].
Objectives
In this study, the aim is to compare and assess the incidence of unplanned uterine curettage between expectant management versus medical and surgical management within of first trimester missed and incomplete miscarriage.
Patients and Methods
Study Design
Description: This study is a randomized controlled trial.
Duration of the study: This study was conducted during a period of 6 months starting from October 2020 till April 2021.
Number of subjects: Totally one hundred and fifty cases were included in this study.
Study setting: This study was conducted at Ain Shams University Maternity Hospital.
Randomization and blinding: The recruited patients in this study will be randomized according to a computer-generated random sequence into two major groups; expectant management (group A), medical (group B) and surgical management (group c) which is control.
Sample Justification: Depending on Trinder et al., [10] who found the frequencies of unplanned curettage in surgical, expectant and medical groups were 5.0%, 44.0% and 13.0% respectively. adjusting the power= 0.80 and α=0.050, and by using PASS 11th release the minimal sample size for an equal size two-arms study to achieve significant difference between each of surgical & medical groups and expectant group is 45 cases in each group (sum will be 90). We will recruit 50 cases in each group (sum will be 150) for possible attrition and further analysis.
Study subjects
Subjects of this study were recruited according to the inclusion and exclusion criteria as following:
Inclusion criteria:
a) Age: between 20-30 years old
b) BMI between 20-25 kg/m2
c) Women with a pregnancy of less than 13 weeks’ gestation who had been diagnosed as having early fetal/embryonic demise (we defined early embryonic demise as an intact gestation sac of greater than 20 mm mean
diameter with no other internal structures and early fetal demise as a fetus of over 7 mm crown-rump length with no heart activity on transvaginal ultrasound scan) and incomplete miscarriage (we defined incomplete miscarriage as areas of mixed echogenicity within the uterine cavity with or without a disordered gestation sac).
Exclusion criteria:
a) Severe hemorrhage or pain to avoid hypovolemic or neurogenic shock history of trauma or surgery during the current pregnancy.
b) Pyrexia above 37.5°C.
c) Severe asthma, hemolytic disease or blood dyscrasias to prevent surgical complications and the risk asthma exacerbation
d) Positive inflammatory parameters (leukocytosis with neutrophilia and positive polymerase chain reaction) to exclude patients with systemic infection or viral hepatitis
e) Thrombocytopenia (< 100 000 per mm3), Current anticoagulation, anemia (hemoglobin<10 g/dl) to prevent haemorrhage
f) Large leiomyomata distorting uterine cavity
g) Systemic corticosteroid treatment due to compromised immunity and liability for infection.
h) Twin or higher order pregnancy to avoid risk of single fetal demise.
Recruitment and procedures applied in the study
• Place of recruitment (place of conduction of the study): subjects were recruited from Ain Shams University Maternity Hospital
• Research Ethics Committee Approval and Quality Control: the protocol and all corresponding documents were declared for Ethical and Research approval by the Council of OB/GYN Department, Ain-Shams University. Furthermore, the approval of the study protocol was granted by Ethics Research Committee (ERC), Faculty of Medicine, Ain-Shams University (ASU).
• Subjects consent: all subjects, were informed about the details of the study, the risks and the benefits, and were all asked to give their consent before the start of the study.
• Procedures applied in the study: All participating women included in this study received a specific information sheet, and an emergency telephone number. Participants were managed according to their computer generated randomized group. The expectant management group was allowed home with no intervention until week 8.
In the medical management, women with incomplete miscarriage or early fetal or embryonic demise received a single vaginal dose of 800 μg misoprostol that was if necessary, repeated twice with a 3 hour interval.
A surgical evacuation of uterine content of conception was offered if expulsion of retained products after expectant management or medical management was not complete. Women in the surgical management group were admitted for surgical suction curettage under general anaesthesia. There was no prophylactic antibiotics used at the time of curettage. All procedures were performed by well-experienced staff of Ain Shams university maternity hospital.
Patients of all groups were informed of the need to return for follow-up surveillance at scheduled hospital visits at 14 days and 8 weeks after the time of diagnosis.
Patients of the expectant group were asked to report any vaginal haemorrhage, discharge and fever; to avoid bathing and vaginal sexual intercourse while vaginal haemorrhage persisted; and to contact the hospital at any time if they experienced excessive vaginal bleeding, severe abdominal pain, fever, or foul-smelling vaginal discharge. If these complications occurred, the patients were admitted to hospital to undergo surgical curettage. Participants have the freedom to decide to leave the study at any time.
In all groups, full blood count was done. Rhesus negative women were offered 250 IU of anti-D irrespective of their allocated management. A follow-up appointment was arranged 14 days for a transvaginal ultrasound scan, full blood count, consultation with the study nurse, and examination by a gynaecologist if symptoms of infection were present. Retained products of conception were diagnosed if areas of mixed echogenicity within the uterine cavity are seen. A surgical curettage was offered if retained products of conception were present. Another follow-up appointment was arranged 8 weeks after trial entry.
The three groups were compared regarding different criteria including
1) The Demographic characteristics of the participants in this study were recorded including their mean age, gestational age, parity, type of miscarriage, bleeding at entry and pain, previous miscarriages, previous surgical evacuation.
2) Primary clinical outcome in the expectant, surgical and medical groups included the incidence of hospital re-admission for unplanned uterine curettage.
3) Secondary clinical outcomes included
a) Documenting the incidence of gynaecological infection within 14 days and 8 weeks (the gynaecological infection defined as two or more of purulent vaginal discharge, pyrexia (above 38°C), and tenderness over the uterus on abdominal examination, and a white blood cell count above 15X 109/L).
b) The treatment with antibiotics for presumed gynaecological infection within 14 days and eight weeks.
c) The duration of clinical symptoms (pain, additional analgesia, vaginal bleeding).
d) Complications (fall in hemoglobin at 10-14 days, blood transfusion, unplanned consultations or admissions within 14 days and within eight weeks).
e) Efficacy (defined as a successful outcome as no unplanned surgical curettage within eight weeks.
Statistical Analysis
The collected data were coded, tabulated, and statistically analyzed using Statistical Package for Social Sciences IBM SPSS® statistics (Statistical Package for Social Sciences) software version 22.0, IBM Corp., Chicago, USA, 2013. The differences between the groups were expressed as risk differences with 95% confidence intervals. Descriptive statistics were done for quantitative data as minimum & maximum of the range as well as mean ± SD (standard deviation) for quantitative normally distributed data, while it was done for qualitative data as number and percentage.
Inferential analyses were done for quantitative variables using Shapiro-Wilk test for normality testing, independent t-test in cases of two independent groups with normally distributed data. In qualitative data, inferential analyses for independent variables were done using Chi square test for differences between proportions and Fisher’s exact test for variables with small expected numbers. Long rank test was used to compare rates. The level of significance was taken at P value<0.050 is significant, otherwise is non significant. Intervention values were calculated as follows:
• Rate elevation=Study Rate - Control Rate
• Efficacy = (Study Rate - Control Rate)/Study rate
• Relative Rate = Study Rate/Control Rate
• Number needed to treat = 1/(Study Rate - Control Rate)
Results
Tab. 1. shows no statistical significant difference (p value > 0.05) between studied groups as regard demographic data (age, BMI and parity). Fig. 1. shows the flow chart of studied cases.
| Variables | Groups | Stat. test | p value | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Expect (n = 50) | Medical (n = 50) | Surgical (n = 50) | |||||||
| Age (years) | Mean ±SD | 26.2 ± 1.9 | 26.5 ± 2.1 | 25.9 ± 1.9 | F = 1.24 | 0.290 N | |||
| Range | 22 - 30 | 20 – 30 | 20 – 29 | ||||||
| BMI (kg/m2) | Mean ±SD | 23.3 ± 0.9 | 22.9 ± 1.4 | 23.1 ± 0.8 | F = 1.97 | 0.142 NS | |||
| Range | 21.6 - 25 | 19.8 – 25 | 21.5 – 25 | ||||||
| Parity | Null | 21 | 42% | 23 | 46% | 23 | 46% | Χ2 = 0.21 | 0.898 NS |
| Parous. | 29 | 58% | 27 | 54% | 27 | 54% | |||
Tab. 1. Comparisons between studied groups as regard demographic data.
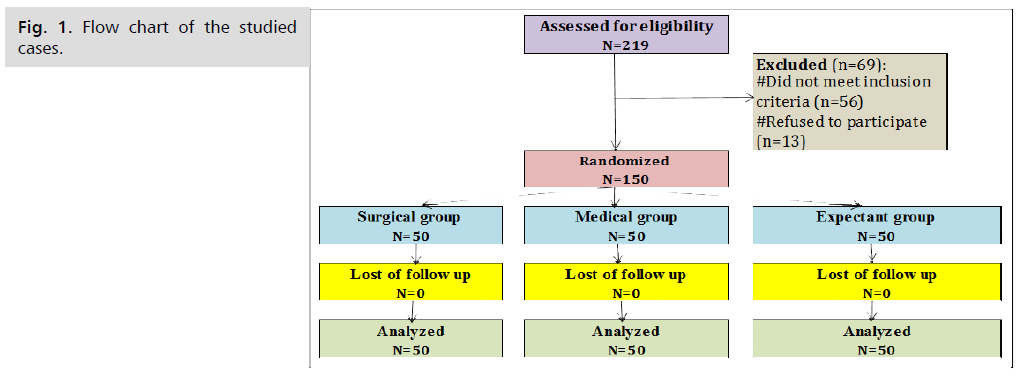
Fig 1. Flow chart of the studied cases.
Tab. 2. Shows no statistical significant difference (p value > 0.05) between studied groups as regard gestational age, type and pain. Statistically significant difference (p value<0.05) between studied groups as regard vaginal bleeding.
| Variables | Groups | Stat. test | p value | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Expect (n = 50) | Medical (n = 50) | Surgical (n = 50) | |||||||
| G. Age (weeks) |
Mean±SD | 8.8 ± 1.75 | 9.16 ± 1.8 | 9.16 ± 1.6 | F = 0.65 | 0.520 NS | |||
| Range | 06-12 | 06-12 | 06-12 | ||||||
| Type | Incomp. | 34 | 68% | 35 | 70% | 37 | 74% | Χ2 = 0.45 | 0.798 NS |
| Missed | 16 | 32% | 15 | 30% | 13 | 26% | |||
| Bleeding | No | 18 | 36% | 20 | 40% | 8 | 16% | Χ2 = 7.77 | 0.02 S |
| Yes | 32 | 64% | 30 | 60% | 42 | 84% | |||
| Pain | No | 30 | 60% | 26 | 52% | 19 | 38% | Χ2 = 4.9 | 0.084 NS |
| Yes | 20 | 40% | 24 | 48% | 31 | 42% | |||
Tab. 2. Comparisons between studied groups as regard Miscarriage characteristics.
Tab. 3. shows highly statistical significant difference (p value<0.001) between studied groups as regard Duration of post-intervention bleeding (days). It was longer in expectant group (12.8 ± 3.6 days) than medical group (8.6 ± 3.1 days) and least in surgical group (7.8 ± 2.9 days).
| Variables | Groups | Stat. test | p value | |||
|---|---|---|---|---|---|---|
| Expect (n = 50) |
Medical (n = 50) |
Surgical (n = 50) |
||||
| Duration (days) | Mean ±SD | 12.8 ± 3.6 | 8.6 ± 3.1 | 7.8 ± 2.9 | F = 34.01 | <0.001HS |
| Range | 5-19 | 3-16 | 3-14 | |||
Tab. 3. Comparisons between studied groups as regard Duration of post-intervention bleeding (days).
Tab. 4. shows statistically significant difference (p value<0.05) between studied groups as regard failed treatment. No statistical significant difference (p value > 0.05) between studied groups as regard reasons.
| Variables | Groups | Stat. test | p-value | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Expect (n = 50) | Medical (n = 50) | Surgical (n = 50) | |||||||
| Failed treatment | No | 37 | 74% | 44 | 88% | 49 | 98% | Χ2 = 17.04 | 0.002 S |
| Yes | 13 | 26% | 6 | 12% | 1 | 2% | |||
| Reasons | Bleeding | 7 | 53.80% | 3 | 50% | 1 | 100% | Χ2 = 0.88 | 0.642 NS |
| Retained products of conception (RPOC) | 6 | 46.20% | 3 | 50% | 0 | 0% | |||
Tab. 4. Comparisons between studied groups as regard failed treatment.
Tab. 5. shows no statistical significant difference (p value > 0.05) between studied groups as regard urgent unplanned D&C.
| Variables | Groups | Stat. test | p value | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Expect (n = 50) | Medical (n = 50) | Surgical (n = 50) | |||||||
| Urgent unplanned D & C | No | 49 | 98% | 47 | 94% | 49 | 98% | Χ2 = 1.65 | 0.437 NS |
| Yes | 1 | 2% | 3 | 6% | 1 | 2% | |||
Tab. 5. Comparisons between studied groups as regard unplanned urgent D&C.
Tab. 6. shows no statistical significant difference (p value > 0.05) between studied groups as regard continued same treatment.
| Variables | Groups | Stat. test | p value | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Expect (n = 50) | Medical (n = 50) | Surgical (n = 50) | |||||||
| Cont. same ttt | No | 48 | 96% | 49 | 98% | 50 | 100% | Χ2 = 2.04 | 0.360 NS |
| Yes | 2 | 4% | 1 | 2% | 0 | 0% | |||
Tab. 6. Comparisons between studied groups as regard continued same treatment.
Tab. 7. shows highly statistical significant difference (p value<0.001) between studied groups as regard shift to surgery, it was more in expectant group than medical group. No statistical significant difference (p value<0.001) between studied groups as regard reasons.
| Variables | Groups | Stat. test | p value | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Expect (n = 50) | Medical (n = 50) | Surgical (n = 50) | |||||||
| Shift to surgery | No | 40 | 80% | 48 | 96% | 50 | 100% | X² = 15.2 | <0.001HS |
| Yes | 10 | 20% | 2 | 4% | 0 | 0% | |||
| Reasons | Bleeding | 6 | 60% | 1 | 50% | - | - | Χ2 = 0.069 | 0.793 NS |
| Retained products of conception (RPOC) | 4 | 40% | 1 | 50% | - | - | |||
Tab. 7. Comparisons between studied groups as regard shift to surgery.
Tab. 8. shows highly statistical significant difference (p value<0.001) between studied groups as regard hypotension. It was more in medical group (14 patients 28%) than expectant group (8 patients 16%) and surgical group (1 patient 2%). No statistical significant difference (p value<0.001) between studied groups as regard haemorrhagic group and sepsis.
| Variables | Groups | Stat. test | p value | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Expect (n = 50) | Medical (n = 50) | Surgical (n = 50) | |||||||
| Hypotension | No | 42 | 84% | 36 | 72% | 49 | 48% | Χ2 = 13.04 | <0.001HS |
| Yes | 8 | 16% | 14 | 28% | 1 | 2% | |||
| Hemorrhagic shock | No | 49 | 98% | 47 | 94% | 50 | 100% | Χ2 = 3.59 | 0.166 NS |
| Yes | 1 | 2% | 3 | 6% | 0 | 0% | |||
| Sepsis | No | 49 | 98% | 50 | 100% | 50 | 100% | Χ2 = 2.01 | 0.365 NS |
| Yes | 1 | 2% | 0 | 0% | 0 | 0% | |||
Tab. 8. Comparisons between studied groups as regard complications.
Tab. 9. shows highly statistical significant difference (p value<0.001) between studied groups as regard hemoglobin difference. It was higher in expectant group (1.2 ± 0.3 g/dl) than medical group (1.03 ± 0.6 g/dl) and surgical group (0.78 ± 0.23 g/dl).
| Variables | Groups | Stat. test | P-value | |||
|---|---|---|---|---|---|---|
| Expect (n = 50) | Medical (n = 50) | Surgical (n = 50) | ||||
| Hb diff (g/dl) | Mean ±SD | 1.2 ± 0.3 | 1.03 ± 0.6 | 0.78 ± 0.23 | F = 15.7 | <0.001HS |
| Range | 0.6 - 2.5 | 0.4 - 2.8 | 0.4 - 1.8 | |||
Tab. 9. Comparisons between studied groups as regard haemoglobin difference.
Discussion
Uterine curettage was traditionally and still commonly performed after incomplete or missed miscarriage. Surgical evacuation of the retained products of conception is occasionally associated with many side effects like: anaesthetic complications, infection, uterine perforation, bowel injury and Asherman’s syndrome [11-14]. Expectant management which allows for the spontaneous passage of retained products of conception was indicated in several studies to be efficient and safe. However, other studies preferred medical management over expectant management after first trimester incomplete miscarriage [15,16].
The aim of our study was to compare and assess the incidence of unplanned uterine curettage between expectant management versus medical and surgical management in the first trimester missed and incomplete miscarriage.
This Randomized controlled trial included 150 patients diagnosed with early fetal demise at less than 13 weeks’ gestation. They were recruited and assessed for eligibility from Ain Shams University Maternity Hospital. Cases were randomized according to a computer-generated random sequence into three groups; Expectant, Surgical and Medical groups.
Our results indicated no significant difference between the studied groups regarding demographic characteristics; age, BMI and parity and no significant difference between the studied groups regarding miscarriage characteristics including the gestational age at the time of miscarriage, type of miscarriage and pain as a symptom of miscarriage (P>0.05). Our results indicated statistically significant difference (P<0.05) between studied groups as regard vaginal bleeding as a symptom of miscarriage.
Such findings were in agreement with a randomized controlled trial by Nadarajah et al., that compared the expectant management versus surgical evacuation of early pregnancy loss on 360 women and indicated no statistically significant difference between the randomized surgical and expectant groups in study characteristics including age, parity, gestational age and type of the miscarriage [17].
Regarding the post-intervention bleeding duration per days among the studied groups, our results indicated that bleeding duration was highly significant and the longest among the expectant group followed by the medical then the surgery groups (P<0.001).
Such findings were in agreement with a randomized prospective study by Al-Ma’ani et al., that studied the expectant versus surgical management of first-trimester miscarriage on 234 women and revealed that bleeding duration was significantly higher among patients following the expectant management in comparison with the surgical management [18].
In explanation of our findings, a retrospective cohort study by Wada et al., on 640 patients who had spontaneous or artificial miscarriage at less than 22 weeks of gestation indicated that compared with the control group, heavy bleeding (> 500 mL) at miscarriage was caused by the retained products of conception hypervascularity that were more frequently observed in the expectant management group and required additional interventions [19].
In agreement with our findings, the study by Nadarajah et al., indicated that the mean duration of bleeding was longer among patients in the expectant group in comparison with the surgical group and the mean total estimated blood loss was 148 ml in the surgical group and 171 ml in the expectant group with a mean difference of 23 ml, which was statistically significant (p<0.01) but not clinically significant [17].
Like our results, a systematic Review by Nanda et al., comparing the expectant care versus surgical treatment for first trimester miscarriage revealed that patients who choose expectant management over uterine aspiration experience more days of bleeding, longer time to completion, and higher rates of unplanned surgical intervention [20].
In agreement with our results, a systemic review by Neilson et al., including three randomized controlled studies including 211 women comparing the medical and surgical management of first trimester miscarriage indicated that patients treated with misoprostol had significantly more days of vaginal bleeding in comparison with those treated with surgery [21].
Our results indicated the presence of statistically significant difference (p-value<0.05) between studied groups as regard failed treatment and shift to surgery that was more prevalent in the expectant group followed by the medical group. There was no statistical significant difference (p-value > 0.05) between studied groups as regard reasons.
Such results were in agreement with Wada et al., study that indicated that although expectant management was successful in 80 % of patients, some patients required additional intervention due to the heavy bleeding at miscarriage and retained products of conception hypervascularity [19].
Like our findings, Trinder et al., study revealed that the main reasons after expectant management included patient request and retained products on scan, moreover, the main reasons after medical management was retained products on scan [10].
In agreement with our findings, a randomized trial by Shelley et al., on 40 patients with first trimester incomplete miscarriage revealed that medical and expectant management were slightly less effective than surgical management, but both were highly effective approaches for the care of women following a first trimester spontaneous miscarriage, with around 80% of women in each group requiring no further intervention to evacuate retained products [22].
Our results selected patients with miscarriage less than 13 weeks gestation to undergo expectant management, such approach was in agreement with a prospective study by Sajan et al., on 112 patients with ultrasonography confirmed pregnancy miscarriages of less than 13 weeks, who were allocated to expectant management that indicated that expectant management showed a decrease in success rate with increase in gestational age so, the selection of patients for expectant management needs to be adjusted according to gestational age [5].
Our results indicated no statistical significant difference between studied groups (expectant, medical and surgical groups) as regard emergency unplanned D&C due to heavy bleeding (p-value > 0.05).
Such findings were in agreement with a prospective observational study by Casikar et al., on 282 women that demonstrated a low rate of unplanned surgical management in women undergoing expectant management for first-trimester miscarriage and revealed that expectant management based on the 2-week rule is a viable and safe option for women with first-trimester miscarriage. However, the same study demonstrated that expectant management longer than 2 weeks without intervention does not confer a greater chance of successful resolution [23].
In disagreement with our finding, a prospective study by Sajan et al., included 112 patients with ultrasonography confirmed pregnancy miscarriages of less than 13 weeks who were assigned to expectant management indicated that the unplanned admissions and emergency evacuation rate was significantly high in expectant management group in comparison with surgical management group [5].
Unlike our finding, a randomized open-label trial by Torre et al., [24] on 182 women diagnosed with spontaneous miscarriage before 14 weeks' gestation indicated that following the expectant management of first-trimester miscarriage increases the rate of unplanned surgical uterine evacuation. Additionally, a randomized controlled trial by Nadarajah et al., revealed that women with expectant management should be prepared for the possibility of surgical intervention because of the higher rates of retained placenta [17].
In disagreement with our findings, a randomized controlled trial by Trinder et al., including 399 to expectant management, 398 to medical management and 403 to surgical management comparing medical and expectant management with surgical management of first trimester miscarriage indicated that expectant management was significantly higher risk of urgent unplanned admission in comparison with surgical and medical managements [10].
As regard shift to surgery, our results indicated a highly statistical significant difference (p-value<0.001) between studied groups as regard shift to surgery; it was more in expectant group than medical group. No statistical significant difference between studied groups as regard reasons. Regarding continued same treatment, our results indicated no statistical significant difference (p-value > 0.05) between studied groups.
Such findings were in agreement with a randomized controlled study by Abdelaleem et al., on 84 patients with a first-trimester miscarriage that indicated that a significantly higher numbers of patients in the expectant group were shifted to surgical evacuation after failed achievement of complete miscarriage at four weeks in comparison with medical group [25].
In agreement with our findings, a study by Schreiber et al., indicated that women who switched their management choice from expectant management to surgical management often did so in reaction to their dissatisfaction with the length of time required to receive a definitive pregnancy loss diagnosis [26].
In disagreement with our results, a randomized controlled trial comparing medical and expectant management of first trimester miscarriage by Bagratee et al., on 131 patients indicated that the complete miscarriage rate was achieved quicker in the medical group than the expectant group by day 1 and that more women in the medical management group would elect the same treatment in the future [27].
Our results indicated a highly statistical significant difference (p value<0.001) between studied groups as regard hypotension. It was more prevalent in medical group (28%) followed by the expectant group (16%) then the surgical group (2%). Our results indicated no statistical significant difference (p value > 0.001) between studied groups as regard the incidences of severe haemorrhage and sepsis.
Such findings were in agreement with an open-labeled randomized clinical trial by Ali et al., on 88 patients with that indicated that side effects are more common in misoprostol management group that included diarrhea, nausea/vomiting, shivering, abdominal pain and vaginal bleeding that could lead to hypotensive symptoms (15). Additionally, a randomized controlled trial by Fernlund et al., indicated that misoprostol treatment is associated with more pain than is expectant management [8].
A retrospective study by Serdinšek et al., on 390 patients diagnosed with missed miscarriage or anembryonic pregnancy indicated that higher beta-hCG values 14 days after medical management and the absence of evacuation of products of conception during hospitalization were associated with a higher complication rate [28].
Our findings were in agreement with a quasi-experimental study compared the side effects of surgical versus expectant managements by Jaffar, that included 50 patients with first trimester incomplete miscarriage and found no significant differences between both groups regarding complications including infection and excessive bleeding [29].
In disagreement with our findings, a prospective clinical study by Banyan et al., that included 50 patients indicated no significant differences regarding the systolic and diastolic blood pressure before and after treatment with misoprostol in patients with first trimester spontaneous incomplete or missed miscarriage [30].
Our results indicated a highly statistical significant difference (p value<0.001) between studied groups as regard hemoglobin difference. It was higher in expectant group (1.2 ± 0.3 g/dl) than medical group (1.03 ± 0.6 g/dl) and surgical group (0.78 ± 0.23 g/dl).
Such findings were in agreement with Wijesinghe et al., which indicated that a minority of patients who were managed expectantly may experience heavy bleeding and drop in hemoglobin that might require hospital admission [31].
Such finding was in disagreement with a randomized controlled trial by Kong et al. that included 180 patients suffering first trimester miscarriage and indicated no significant differences between the surgical, medical and expectant groups regarding the drop in haemoglobin level [32].
A like our findings, a prospective, randomized study by Patua et al., on 100 patients with incomplete first trimester miscarriage that indicated no significant differences between the medical and surgical management groups regarding the pre- and post-treatment difference in mean hemoglobin [33].
Conclusion
The incidence of failed treatment and shift to surgery after expectant, medical and surgical management of spontaneous first trimester miscarriage was more prevalent in the expectant group followed by the medical group then the surgical group. Regarding complications, our results indicated a highly statistical significant difference between studied groups as regard hypotension. It was more prevalent in medical group followed by the expectant group then the surgical group. There was no statistical significant difference between studied groups as regard the incidences of severe haemorrhage, unplanned emergency curettage and sepsis.
Authors Contribution
(A) Study Design · (B) Data Collection . (C) Statistical Analysis · (D) Data Interpretation · (E) Manuscript Preparation · (F) Literature Search · (G) No Fund Collection
References
- Webster K, Eadon H, Fishburn S, et al. Ectopic pregnancy and miscarriage: diagnosis and initial management: summary of updated NICE guidance. BMJ. 2019;367.
- Rafi J, Khalil H. Expectant management of miscarriage in view of NICE Guideline 154. J Pregnancy. 2014;2014.
- Salazar CA, Isaacson K, Morris S. A comprehensive review of Asherman's syndrome: causes, symptoms and treatment options. Curr Opin Obstet Gynecol. 2017;29(4):249-56.
- Cubo Nava A, Soto Pino ZM, Haro Pérez AM, et al. Medical versus surgical treatment of first trimester spontaneous abortion: A cost-minimization analysis. PloS one. 2019;14(1):e0210449.
- Sajan R, Pulikkathodi M, Vahab A, et al. Expectant versus surgical management of early pregnancy miscarriages-A prospective study. J Clin Diagnostic Res. 2015(10):QC06.
- Chu J, Hardy P, Beeson L, et al. What is the best method for managing early miscarriage?. BMJ. 2020;368.
- Sajadi-Ernazarova KR, Martinez CL. Abortion complications. InStatPearl. StatPearls Publishing. 2021.
- Fernlund A, Jokubkiene L, Sladkevicius P, et al. Misoprostol treatment vs expectant management in women with early non‐viable pregnancy and vaginal bleeding: a pragmatic randomized controlled trial. Ultrasound Obstet Gynecol. 2018. 51 (1); 24-32.
- Kushwah B, Kushwah DS. A randomized controlled study on expectant management of incomplete abortions caused by self-medication. Int J Basic Clin Pharmacol. 2019. 8(6); 1409-1412.
- Trinder J, Brocklehurst P, Porter R, et al. Management of miscarriage: expectant, medical, or surgical? Results of randomised controlled trial (miscarriage treatment (MIST) trial). BMJ. 2006;332(7552):1235-40.
- Kaur R, Gupta K. Endocrine dysfunction and recurrent spontaneous abortion: An overview. Int J Appl Basic Med Res. 2016;6(2):79.
- Tsur A, Malvasi A, Vergari U, et al. Spontaneous Abortion Complications. InManagement and Therapy of Early Pregnancy Complications. Springer, Cham. 2016;.29-50.
- Kong GW, Lok IH, Yiu AK, et al. Clinical and psychological impact after surgical, medical or expectant management of first‐trimester miscarriage–a randomised controlled trial. Aust N Z J Obstet Gynaecol. 2013;53(2):170-7.
- Hooker AB, Aydin H, Brölmann HA, et al. Long-term complications and reproductive outcome after the management of retained products of conception: a systematic review. Fertil Steril. 2016;105(1):156-64.
- Ali S, Majid S, Ali MN, Taing S, Rehman MU, Arafah A. Cytokine imbalance at materno-embryonic interface as a potential immune mechanism for recurrent pregnancy loss. Int Immunopharmacol. 2021;90:107118.
- Tzur Y, Samueloff O, Raz Y, et al. Conception rates after medical versus surgical evacuation of early miscarriage. Fertil Steril. 2021;115(1):118-24.
- Nadarajah R, Quek YS, Kuppannan K, et al. A randomised controlled trial of expectant management versus surgical evacuation of early pregnancy loss. Eur J Obstet Gynecol Rep Biol. 2014;178:35-41.
- Al-Ma’ani W, Solomayer EF, Hammadeh M. Expectant versus surgical management of first-trimester miscarriage: a randomised controlled study. Arch Gynecol Obstet. 2014;289(5):1011-5.
- Wada Y, Takahashi H, Suzuki H, et al. Expectant management of retained products of conception following abortion: A retrospective cohort study. Eur J Obstet Gynecol Rep Biol. 2021;260:1-5.
- Nanda K, Lopez LM, Grimes DA, et al. Expectant care versus surgical treatment for miscarriage. Cochrane Database Syst Rev. 2012(3).
- Neilson JP, Gyte GM, Hickey M, et al. Medical 226 treatments for incomplete miscarriage (less than 24 weeks). 227 Cochrane Database Syst Rev. 2010 (1): CD007223.
- Shelley JM, Healy D, Grover S. A randomised trial of surgical, medical and expectant management of first trimester spontaneous miscarriage. Aust N Z J Obstet Gynaecol. 2005;45(2):122-7.
- Casikar I, Bignardi T, Riemke J, et al. Expectant management of spontaneous first‐trimester miscarriage: prospective validation of the ‘2‐week rule’. Ultrasound Obstet Gynecol. 2010;35(2):223-7.
- Torre A, Huchon C, Bussieres L, et al. Immediate versus delayed medical treatment for first-trimester miscarriage: a randomized trial. Am J Obstet Gynecol. 2012;206(3):215-e1.
- Abdelaleem Ma, Ali Mk, Emam S, et al. Medical Versus Expectant Management In Women With Incomplete First-Trimester Miscarriage Initially Treated With Misoprostol: A Randomized Controlled Study. Fertil Steril. 2020;114(3):E46.
- Schreiber CA, Creinin MD, Atrio J, et al. Mifepristone pretreatment for the medical management of early pregnancy loss. N Engl J Med. 2018;378(23):2161-70.
- Bagratee JS, Khullar V, Regan L, et al. A randomized controlled trial comparing medical and expectant management of first trimester miscarriage. Hum Reprod. 2004;19(2):266-71.
- Serdinšek T, Reljič M, Kovač V. Medical management of first trimester missed miscarriage: the efficacy and complication rate. J Obstet Gynaecol. 2019;39(5):647-51.
- Jaffar H. Comparison of Expectant and Surgical Management of Incomplete First-Trimester Miscarriage. Ann Pak Inst Med Sci. 2013;9(1):33-7.
- Banyan NA, Saleh A, Salih SA, et al. Single Vaginal Dose of 800 μg Misoprostol for Termination of First Trimester Spontaneous Incomplete or Missed Miscarriage. Obstet Gynecol Int J. 2015;2(3):00040.
- Wijesinghe PS, Padumadasa GS, Palihawadana TS, et al. A trial of expectant management in incomplete miscarriage. Ceylon Med J. 2011;56(1).
- Kong GW, Lok IH, Yiu AK, et al. Clinical and psychological impact after surgical, medical or expectant management of first‐trimester miscarriage–a randomised controlled trial. Aust N Z J Obstet Gynaecol. 2013;53(2):170-7.
- Patua B, Dasgupta M, Bhattacharyya SK, et al. An approach to evaluate the efficacy of vaginal misoprostol administered for a rapid management of first trimester spontaneous onset incomplete abortion, in comparison to surgical curettage. Arch Gynecol Obstet. 2013 Dec;288(6):1243-8.
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Author Info
Eithar Mohammed*, Tarek Tamara, Sherif Ashoush and Gihan El-HawwaryCopyright:This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.