Research - (2025) Volume 20, Issue 1
Study the effect of some biochemical enzymes at seminal plasma of infertile patients
Majeed Hanan Abbas Al-Zubaidi and Balkees Abd Ali Abd Aun Jwad*Received: 02-Jan-2025, Manuscript No. gpmp-25-157635; Editor assigned: 03-Jan-2025, Pre QC No. P-157635; Reviewed: 23-Jan-2025, QC No. Q-157635; Revised: 30-Jan-2025, Manuscript No. R-157635; Published: 31-Mar-2025
Abstract
Current study included 49 semen samples collected from sub-fertile men, after the abstinence period (3 to 5 days); it was conducted in the laboratory of Al- Imam Al- Hussein at Karbala province for six month from 1/1/2023 to 1/6/2023.
The purpose of this research was to evaluate the correlation between LDH activity in the seminal plasma of infertile men and some sperm parameters, and detected activity level of LDH in different sub-fertile patients. The results revealed significant increase (P<0.05) in oligozoospermia compared to normospermia and Asthenospermic, also revealed a significant negative correlation (PÃÃ??0.05) between progressive motility percent and lactate dehydrogenase activity in asthenozoospermic men.
Concluded: No significant correlation between sperm concentration and lactate dehydrogenase activity, the significance of LDH activity to detecting the capacity of gland function.
Keywords
Lactate dehydrogenase; Seminal plasma; Sperm; Fertility
Introduction
Seminal plasma is a liquid compound, which serves as a medium for moving extrusion spermatozoa from the testis to oocyte in the female reproductive canals [1]. Seminal plasma not only transports the spermatozoa but also equips the protection and nutrition to the spermatozoa in the female reproductive system [2].
Seminal plasma comprises of various biochemical components, such as cholesterol, glucose, proteins, antioxidant, mineral elements and enzymes [3]. These enzymes are vital components of seminal plasma and have important roles in the formation, activity and functions of spermatozoa. The levels of enzymes in the human seminal plasma are very important for the spermatozoal function [4].
One of these enzymes is lactate dehydrogenase enzyme is present in almost cells of the body and create only in the cytoplasm of the cell, the activities of this enzymes are existing in the several organs and tissues [5,6]. Lactate dehydrogenase is a hydrogen transmission enzyme that catalysis the oxidation of L-lactate to pyruvate with Nicotinamide-Adenine Dinucleotide (NAD)+ as hydrogen acceptor, the last step in the metabolic chain of anaerobic glycolysis [7]. Lactate dehydrogenase in the testis has important role because the interaction in the spermatogenesis and the activity of spermatozoa [8]; Also, it is present in the seminal plasma and have main role in providing energy for cell metabolism [9].
Seminal plasma enzymes are interacting with the presence or absence of spermatozoa and male infertility; many studies have been done for assessment of these enzymes activities in the seminal plasma and the relationship with infertility [10]. Male infertility caused by several reasons such as congenital malformations or external factors such as smoking, alcohol, medicines and anabolic steroids, other reasons idiopathic have ratio is about (40-50%) [11]. Infertility patients can be divided into several factors as sperm concentration, motility, and morphological abnormal sperm [12].
Material and Methods
Semen specimens’ collection
The samples were collected from patients via masturbation after 3-5 days of sexual abstinences in the specialized sanitary container, then the specimens liquefy at 37C°, and the seminal fluid analysis was performed to detect the sperm parameters. According to the seminal fluid analysis the infertile patients classified into normospermia 8/49 samples, oligospermia 9/49 samples and asthenospermia 32/49 samples [12].
Sample preparation for examination: One droplet (10 μl) of sample was taken after liquefies and putting on the warm glass slides, covered by cover slip (22×22 Mm) and was examined under 40X power by the light microscope for assessment the sperms parameters which includes sperm concentration, 4ZL sperm percent motility, sperm viability percent, round cell concentration, morphological abnormal sperms and agglutination [12].
Sperm concentration: The concentration was determined from the average of the sperms number in ten random fields and multiplies by the factor 106. The count of sperms calculated by multiplying the concentration with the volume of ejaculate. The patient called oligozoospermia when sperm concentration less than 15 million sperm per ml [12].
Sperm motility: At least 200 sperms were calculated from each sample, then were recorded an average of motile sperms, which owns progressive forward movement, also was examined the percent of the sluggish motile, topical motile and immotile sperms [12].
It was classified according to world health organization and as below:
• A= progressive motility
• B= slow or sluggish progressive motility
• C= Immotile.
LDH assessment
Lactate Dehydrogenase (LDH) activity: The concentration of lactate dehydrogenas enzyme was measured in serum of blood of 49 mens by observing the concentration of lactate was formed from reduced pyruvate by Lactate Dehydrogenase (LDH) at PH 7.4, temperature 30 ºC using colorimetric method according to the manufacture instruction (Randox Laboratories, England)
Pyruvate is reduced to lactate by Lactate dehydrogenase (LDH) at PH 7.4 and at 30 ºC. The progress of the accompanying oxidation of NADH to NAD+ is monitored continuously by measuring the rate of absorbance decrease at 340 nm in a
Statistical analysis: It was done by using statistical package for social science (SPSS) (the version 22.0) according to Mallery P, et al. [13].
Results
The estimation of LDH activity in seminal plasma of infertile patients showed significant increase (P<0.05) in oligospermia compared to normospermia and asthenospermia (Fig. 1.).
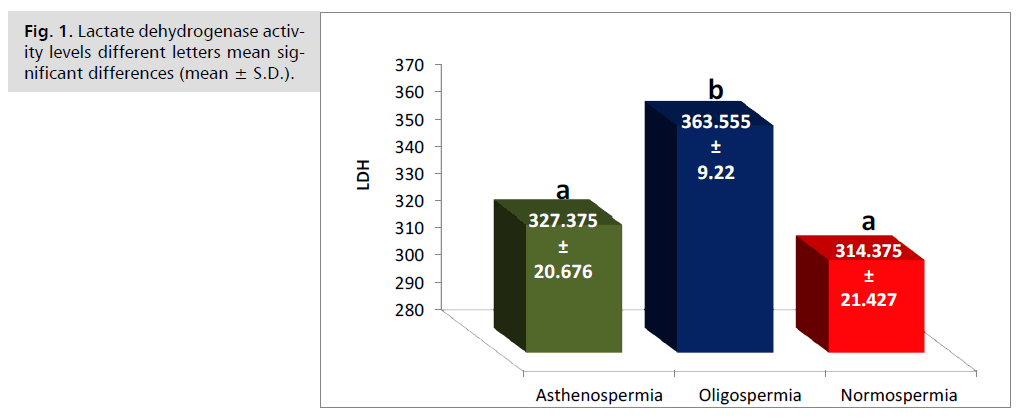
Fig. 1. Lactate dehydrogenase activity levels different letters mean significant differences (mean ± S.D.).
The results revealed positive correlation between progressive motility percent and lactate dehydrogenase activity in the group of oligospermia (Fig. 2.).
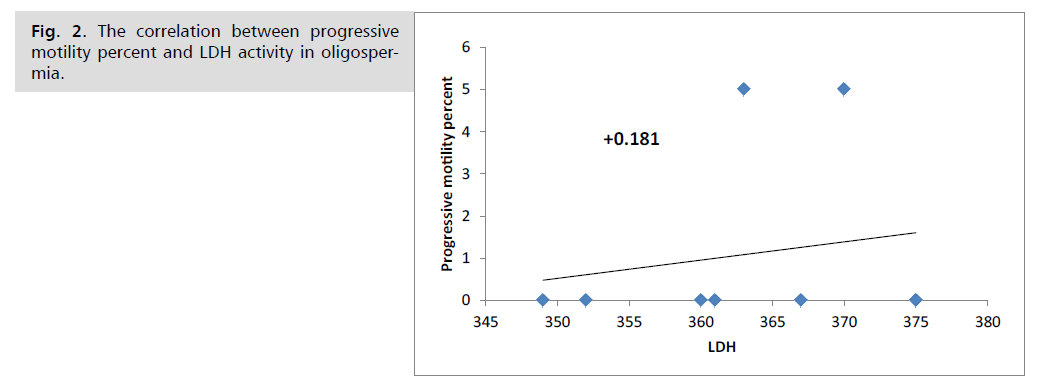
Fig. 2. The correlation between progressive motility percent and LDH activity in oligospermia.
While, results revealed negative correlation between sperm concentration and LDH activity in oligospermic patients (Fig. 3.).
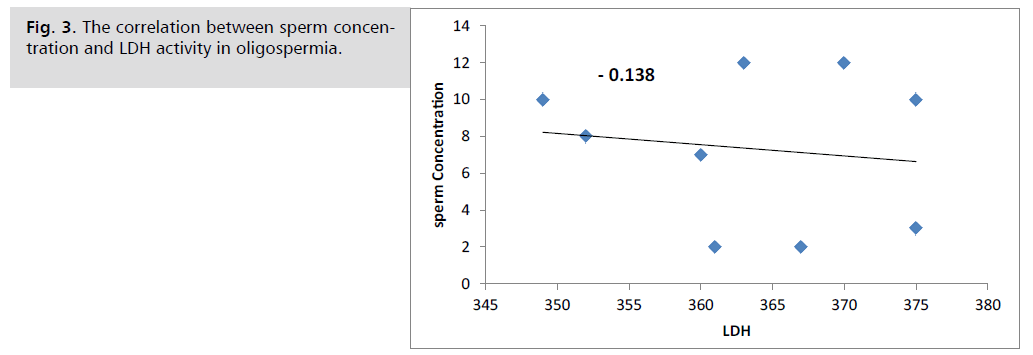
Fig. 3. The correlation between sperm concentration and LDH activity in oligospermia.
Also results showed negative correlation between progressive motility percent and lactate dehydrogenase activity in normospermic men (Fig. 4.).
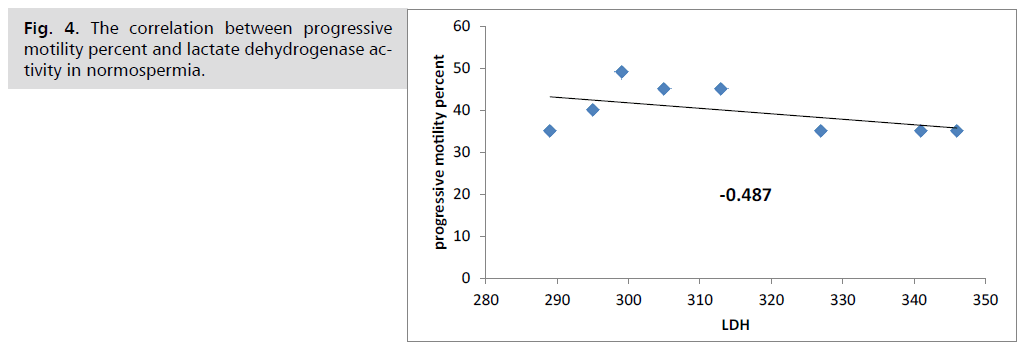
Fig. 4. The correlation between progressive motility percent and lactate dehydrogenase activity in normospermia.
And results showed positive correlation between sperm concentration and lactate dehydrogenase activity in normospermia (Fig. 5.).
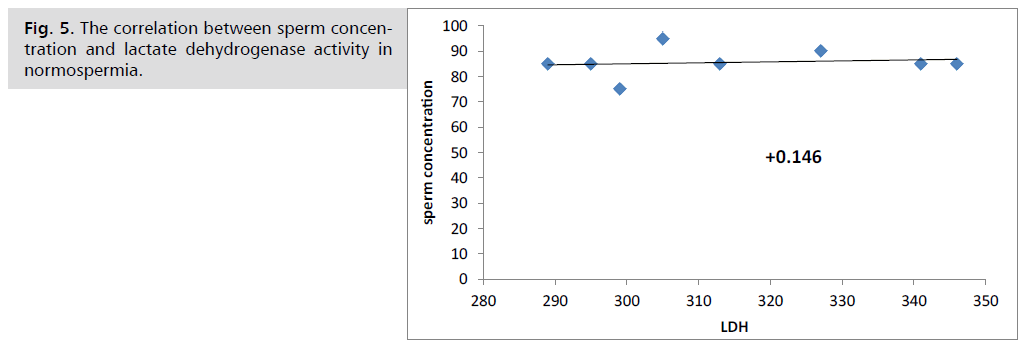
Fig. 5. The correlation between sperm concentration and lactate dehydrogenase activity in normospermia.
The results revealed significant negative correlation between progressive motility percent and lactate dehydrogenase activity in asthenospermic men (Fig. 6.).
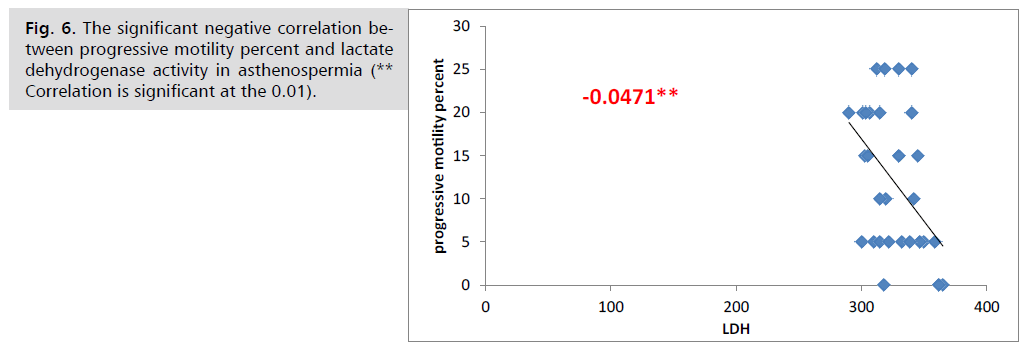
Fig. 6. The significant negative correlation between progressive motility percent and lactate dehydrogenase activity in asthenospermia (** Correlation is significant at the 0.01).
Also results showed negative correlation between sperm concentration and lactate dehydrogenase in asthenospermic patients (Fig. 7.).
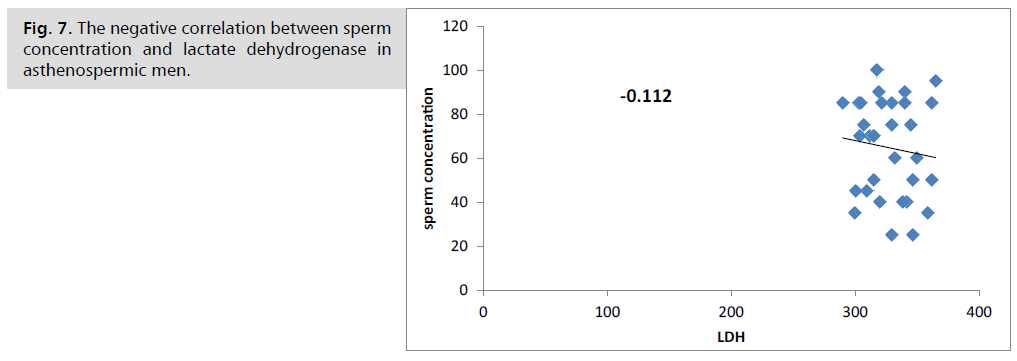
Fig. 7. The negative correlation between sperm concentration and lactate dehydrogenase in asthenospermic men.
Discussion
The results of current study shown significant increase (P<0.05) of LDH activity in seminal plasma of infertile patients in oligospermia compared to normospermia and asthenospermia (Fig. 1.), that may be refer to the normal activity of prostate secretion in normospermic and asthenospermic men, but in patients of oligospermia, the increment of LDH activity may be refer to the increasing in the percentage of live and normal sperm corresponded to an increasing in LDH activity in the seminal fluid. It has been stated that LDH plays an important metabolic role in sperm capacitation and fertilization [14]. Amadou CF, et al. [10] revealed non-significant differences (P<0.05) between seminal plasma LDH activity of normozoospermia and azoospermia.
The results revealed positive correlation between progressive motility percent and lactate dehydrogenase activity in the group of oligospermia (Fig. 2.), but it was showed negative correlation between progressive motility percent and lactate dehydrogenase activity in normospermic men (Fig. 4.), also it was showed significant negative correlation between progressive motility percent and lactate dehydrogenase activity in asthenospermic men (Fig. 6.), that may refer to reduction in prostate secretion, or because the decrease of LDH activity by conversion from active shape to other with less activity, that effect on sperm count and motility. Asadpour R [14] and Goldberg E [15] observed the significant correlations were found between LDH levels and rat sperm viability, also mention every increase in the percentage of live and normal sperm corresponded to an increase in LDH activity in the seminal fluid. It has been stated that LDH plays an important metabolic role in sperm capacitation and fertilization [16].
Fig. 5. revealed positive correlation between sperm concentration and lactate dehydrogenase activity in normospermia, but Fig. 3. revealed negative correlation between sperm concentration and LDH activity in oligospermic patients, also results showed negative correlation between sperm concentration and lactate dehydrogenase in asthenospermic patients ((Fig. 7.), that may refer to function of this enzyme in the semen and effect on the sperm function. Hereng TH, et al. [17] conclude that exogenous pyruvate and glucose together speed up the glycolytic machinery to produce sufficient ATP to support progressive motility and capacitation, or may be refer to prostate secretion and the effect of this enzyme function on regular the semen component. Owen DH, et al. [18] mention several seminal plasma components present in substantial quantities and excluded from studies for many reasons of simplicity and practicality. These include lipids, choline, sialic acid, inositol, ascorbic acid, creatine, and pyruvate.
Conclusion
This study concluded the significance of LDH activity to detecting the capacity of gland function, and no significant correlation between sperm concentration and lactate dehydrogenase activity.
Future Study
• Estimate these enzymes for infertility patients after the seminal fluid analysis.
• 2-Study the effects of seminal plasma enzymes in the female reproductive system on the capacitation, hyper activation and acrosome reaction.
References
- Mann T, Lutwak-Mann C. Male reproductive function and semen: Themes and trends in physiology, biochemistry and investigative andrology. Springer. 2012.
- Schjenken JE, Robertson SA. Seminal fluid and immune adaptation for pregnancy–comparative biology in mammalian species. Reprod Domest Anim. 2014; 49:27-36.
- Juyena NS, Stelletta C. Seminal plasma: An essential attribute to spermatozoa. J Androl. 2012;33:536-551.
- Brooks DE. Biochemistry of the male accessory glands. Marshall’s Physiology of Reproduction. 1990;2:569-690.
- https://www.scirp.org/reference/referencespapers?referenceid=2304721.
- https://www.scirp.org/reference/referencespapers?referenceid=1805648
- https://wwwn.cdc.gov/nchs/data/nhanes/public/2007/labmethods/ld-biopro_e_lx20.pdf
- Blackshaw AW, Elkington JS. Developmental changes in lactate dehydrogenase isoenzymes in the testis of the immature rat. Reproduction. 1970; 22(1):69-75.
- Aydin S, Yilmaz Y, Odabas O, et al. A further study of seminal plasma: Lactate dehydrogenase and lactate dehydrogenase-X activities and diluted semen absorbance.J Forum Euro Clin Chem Soc. 1997;35(4): 261-264.
- Amadou CF, Sylvère NK. Eric A, et al. Comparative Study of Enzymatic Markers in Seminal Liquids of Normospermic and Azoospermic Samples at Pasteur Institute of Cote D’Ivoire (IPCI). Am J Phytomed Clin Therap. 2014; 2(11):1252-1261.
- Jungwirth A, Diemer T, Dohle GR, et al. Guidelines for the investigation and treatment of male infertility. Eur Urol. 2004; 46(5):555-558.
- World Health Organization. WHO laboratory manual for the examination and processing of human semen. WHO. 2021.
- Mallery P, George D. SPSS for windows step by step. Allyn Bacon Inc. 2000.
- Asadpour R. Relationship between mineral composition of seminal plasma and semen quality in various ram breeds. Acta Sci Veterin. 2012; 40(2):1-8.
- Goldberg E. Reproductive implications of LDH-C4 and other testis-specific isozymes. Exp Clin Immunogenet. 1985; 2(2):120-124.
- Duan C, Goldberg E. Inhibition of lactate dehydrogenase C4 (LDH-C4) blocks capacitation of mouse sperm in vitro. Cytogenet Genome Res. 2003; 103(3-4):352-359.
- Hereng TH, Elgstøen KB, Cederkvist FH, et al. Exogenous pyruvate accelerates glycolysis and promotes capacitation in human spermatozoa. Human Reprod. 2011;26(12):3249-3263.
- Owen DH, Katz DF. A review of the physical and chemical properties of human semen and the formulation of a semen simulant. J Androl. 2005;26(4):459-469.
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Author Info
Majeed Hanan Abbas Al-Zubaidi and Balkees Abd Ali Abd Aun Jwad*Copyright:This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.