Research Article - (2025) Volume 20, Issue 3
Pregnancy associated breast carcinoma: A multi-centre study
Basma Hameed Mageed1, Jamal Mohammed Ibrahim2, Awni Ismail Sultan3* and Nisreen Mohammed Ibraheem4Received: 20-Jun-2025, Manuscript No. gpmp-25-165660; Editor assigned: 23-Jun-2025, Pre QC No. P-165660; Reviewed: 15-Jul-2025, QC No. Q-165660; Revised: 23-Jul-2025, Manuscript No. R-165660; Published: 29-Aug-2025
Abstract
Pregnancy Associated Breast Cancer (PABC) is that cancer recorded within pregnancy or within one year of puerperium. It is increasingly reported disorder lately. The clinical presentation and workup are nearly similar to those cases that are not pregnant except some considerations in the management in a maneuver that balances the treatment benefits vs. minimizing risks towards both the mother and her foetus. A group of 62 women who were pregnant or during puerperal phases whom were diagnosed as having breast ca, enrolled in a cohort study. The following data reported about the patients’ demographics, age of diagnosis, and about the tumor in terms of stage, grade, nodal and hormonal status. Then modality of management recorded and paients’ outcome within one year of follow up. We found that 48 (77.4%) cases were pregnant and 14 (22.6%) puerperal women, maternal age at diagnosis was 36.8 years, and of 28.2 weeks gestational age for those pregnant. A 39 (62.9%) of cases had lymph node involvement, 49 (79%) of cases had low grade tumor, 29(46.8%) of cases were at stage 2, besides 55 cases (88.7%) was ductal carcinoma while 7 (11.3%) cases had lobular type. Surgically 56(90.3%) of cases had modified radical mastectomy with axillary lymph node dissection. Most patients 38 (86.4%) postponed chemotherapy after delivery. The aim of the study was to evaluate the prevalence and outcome of pregnancy associated breast carcinoma among different main health centers.
Keywords
Pregnancy-Associated Breast Cancer (PABC); Mastectomy; Chemotherapy; Breast conserving surgery
Introduction
Pregnancy-Associated Breast Cancer (PABC) is globally known as cancer diagnosed during pregnancy period or within twelve months following birth of baby. Therefore, it basically includes two isolated disease items: breast cancer reported at any of the pregnancy trimesters (PrBC) and breast carcinoma discovered within one complete year of the postpartum period (PPBC) [1].
Though rare, pregnancy-associated breast cancer still is the commonest solid mass malignancy notified at the pregnancy era, and accounts for 21% of all malignancies reported in pregnant ladies. Its incidence is 1 in each 1000-3000 pregnancies all over the planet in addition to those figured out within 12 months of delivery [2].
Presentation
Regarding the age of incidence, this specific version of breast carcinoma is not expected to affect elderly in contrast to usual malignant breast neoplasms. As it’s a disease of women of child bearing age, so the majority of cases are relatively young, i.e. not reaching the age of 40 years old. Being outside the range of mammography screening schedules, besides many surgeons are not happy to send such cases for diagnostic mammogram worrying of possible fetal radiation exposure in addition to low accuracy due to dense breast tissue in younger girls with the conception-related physiological changes. This is also may make most of the patients are symptomatic at the moment of presentation [3].
The factors raising the risk of harboring breast ca in pregnancy are similar to usual non-pregnant females, in terms of: early menarche, late menopause, nulliparity, type of meals, weight gain, lifestyle, and other family member exposure [4].
Symptoms are variable from breast or axillary mass, ulcer, skin tethering, nipple inversion, suspicious nipple discharge, while local signs are: unilateral breast lumpiness, edema without or with redness [3].
Sonography is the imaging aid of choice for starting assessment of breast complaints during pregnancy with a sensitivity of nearly 95% in making the diagnoses of conception related ca breast are possible.
Diagnostic mammography once indicated, is safely performed within conception, with a relatively small dose radiation of (200 – 400) mrad, which does not adversely affect embryologic organogenesis. However, its use is limited in pregnancy for risk concerns. When mammogram is required after confirming malignancy, it’s taken with abdominal shielding to lessen radiation effects on the growing foetus [4].
Breast MRI with and without contrast is a beneficial safe diagnostic way for breast carcinoma; it has a sensitivity and specificity of (72-100)% and 89% respectively.
A contrast agent, known as Gadolinium, is sorted as a (category C) pregnancy group. Yet, intravenously introduced gadolinium dependent contrast matter must be omitted because they readily cross the placental circulation.
Metastasis usually goes to the liver parenchyma, spine and lungs. To check for that, a chest roentgenography with foetal protecting shields is done. Other imagings like: CT, P bone scintigraphy or PET scan are never indicated, yet lympho-scintigraphy just prior to sentinel LN biopsy is quite safe for the embryo.
Staging and prognosis is generally the same as in non-pregnant ladies [5].
Treatment of PABC
Treatment cannot be accomplished by just one specialty doctor, and options may include any one or more of the following: surgery, obstetrics, chemotherapy, radio-therapy, and/or hormonally based medications. The decision of starting the treatment needs careful equilibrium between controlling the tumor and reducing unwanted effects to the foetus [6].
Multidisciplinary team MDT should take part in the management plan. Good synergy among surgeons, plastic surgeons, oncologists, obstetricians, and others is vital to build a successful treatment agenda that both defeats cancer and respects the wish of the pregnant lady. Hence, simply the choice of management better to consider the gestational age, the stage of the neoplasm and, the patient’s wishes [3].
Surgery
The spectrum of surgical procedures are so wide, by the way such options used to treat women with PABC are known to be secure and can be accomplished at any pregnancy trimester. We have two options mastectomy and breast- sparing surgery [7].
Nevertheless, half of cases are discovered to have spread to the axillary nodal lymphatics, so surgical dissection is performed. For patients with no metastasis, a SLNB (Sentinel LN Biopsy) is ordered. Before this biopsy widely practiced, the usage of Tc-99m isotope is permitted to localize the first draining node, while stains such as MB methyl blue are discouraged because of the significant risk of anaphylaxis [4].
The surgery option must be dependent upon gestational age, the stage of the lesion and maternal plus her baby hazards. Both foetal and maternal status may be observed during surgery. In regard to functional gestational updates, more care should be considered during intubation, chemoprophylaxis with anti-acids (H2 receptor blockers) and LMW (Low Molecular Weight heparins) must be done and a state of normotension should be kept to safeguard the uterus and placental blood supply [8].
Local complications of surgery include haematoma, dehiscence of incision, delayed healing, bleeding, fat necrosis, nerve injury, flap necrosis or cosmetic deformity.
Safely given medications during pregnancy are: desflurane, propofol, morphine, corticosteroids, lidocaine and ketamine. But nitrous oxide is contra-indicated due to its harmful sequelae on foetal growth and development [9].
Chemotherapy
Chemotherapy is usually indicated to fight breast ca. It may be administered as neo-adjuvant or adjunctive treatment before radiotherapy or postoperatively.
Chemotherapy in Pregnancy related BC cases is permitted in the intermediate and last trimesters due to the likelihood of congenital defects is relatively low, (1.5%–3%), compared to (10–20%) in the first trimester so considered as teratogenic here [10].
But, the onset of initiation can differ according to the stage and sort of the ca and the gestational stage as must to judge fetal risks vs. mother advantages.
From nearly (12–14) weeks of conception, several chemo-therapy items may be securely given. Standard taxanes-anthracyclines based schedules, often used in usual nonpregnant women, can be planned [11].
Studies claim that pharmacokinetics of chemotherapy agents vary through pregnancy, ending in really less medication exposure in comparison to nonpregnant cases. Metabolism in placenta aids in that, resulting in fewer peak plasma levels with a more rapid clearance of these chemical medications.
It’s advised that these medicines to be stopped beyond the 35th weeks of gestation, as they may adversely alter bone marrow physiology and, therefore, blood relevant problems may take place at childbirth [12].
Hormonal treatment
Women with positive ER receptor’s breast cancer may be given hormone-based remedy containing tamoxifen, goserelin and anastrozole [13]. The safety usage of these drugs within childbearing period has not been adequately analyzed and reported, and (except tamoxifen), almost all of them except category X.
Hormonal agents are never used during pregnancy due to the high risk of foetal birth defects, and better withheld till baby birth [14].
Radiation therapy
Radiotherapy as part of the management of Ca breast is a usually used to adjunct treatment, and can be postponed until the post-partum period. On the second hand, it should be ordered when there are precautions to other modalities of treatments [15].
The largest challenge is the risk of foetal exposure to radiation especially while the embryo organs are formed, and involve the occurrence of anatomical malformations, mental delayed development, micro-cephaly, intra-uterine hypotrophy or secondary cancers. The hazard of foetal harm raises once the dosage crosses 0.1 Gy emitted to the fetus [16].
Targeted therapy
Treatment of HER2_ positive cancers is focused upon the trial of trastuzumab (a HER2-targeted mono-clonal Ab), lapatinib (epithelial growth factor) and pertuzumab (humanised monoclonal antibody). The administration of trastuzumab can be stopped till the post-puerperal period due to its teratogenic effect [13].
Supportive care
As a complication of treatment of breast cancer, these side-effects may occur: nausea, vomiting and neutropenia.
For ladies with PABC, the following items might be tried to reduce the above-mentioned unwanted effects: corticosteroids, ondansetron, promethazine, erythropoietin, and granulocyte colony –stimulating factor [14].
Termination of pregnancy
Termination of pregnancy is never a routinely planned decision, as it doesn’t significantly affect the life span of patients. The opinion of the patient should be suitable with her traditions & beliefs [4].
Patients and Methods
Ethical consideration: After obtaining the ethical and legal approval from the health authorities,
Study design: The current study is a descriptive cohort study during the period from February 2018 to December 2024.
Sampling: Convenience sample chosen from patients visited breast clinics, surgical, or obstetrical clinics within Kirkuk, Azadi and Baquba Teaching Hospitals during the period of study. Sample included 62 pregnant women (or in puerperal period) diagnosed as having breast carcinoma. Informed consent was signed after discussed from all of them to make use of their clinical and lab data for this study.
Surgery for most cases included modified radical mastectomy followed by axillary lymphatic ablation. Some selective cases were arranged for a more conservative operation then by irradiation therapy in the puerperal era. Chemo_therapy for most cases were postponed till after delivery according to patient’s demand as they were worried about fetal risks (and few women received full courses before labor) involved the virtual schedule of FEC (5-fluorouracil, epirubicin, and cyclophosphamide),
All patients were followed for one year after surgical operation.
Data collection and analysis: Data collected by direct interview with patients to full a questionnaire that contains questions about sociodemographic information, other factual questions as (age of initial diagnosis, cancer pathology, size, grade, lymph node invasion and ER hormone status were recorded). After that data summarized and presented by tables and suitable figures.
Exclusion criteria: Excluded cases are women with breast cancer recorded after twelve months following child delivery or with deficient informative data.
Results
The results found that, there were 48 (77.4%) pregnant and 14 (22.6%) puerperal women diagnosed as breast Fig. 1.
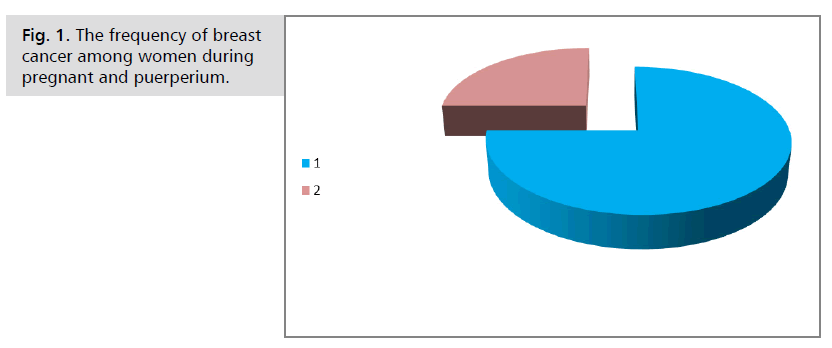
Fig. 1. The frequency of breast cancer among women during pregnant and puerperium.
The result showed that the mean ± SD maternal age at time of breast cancer diagnosis was 36.8 ± 4.1 years. Also, the table showed that mean ± SD of gestational age was 28.2 ± 2.3 weeks at time of diagnosis Tab. 1.
| Variables at time of diagnosis | Mean ± standard deviation |
|---|---|
| Maternal age (Total 62) | 36.8 ± 4.1 year |
| Gestational age (Total 48) | 28.2 ± 2.3 week |
Tab. 1. Some variables at time of breast cancer diagnosis.
This figure showed that 39 (62.9%) of cases had lymph node involvement, while 23 (37.1%) of cases not involved lymph node as in Fig. 2.
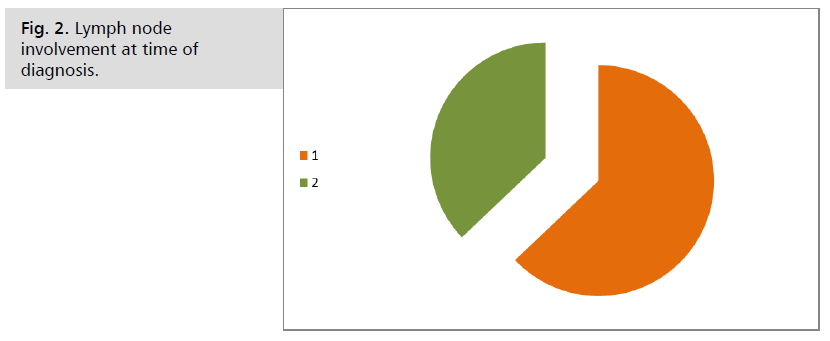
Fig. 2. Lymph node involvement at time of diagnosis.
The results revealed that 49 (79%) of cases had low grade tumor but 13 (21%) of cases with high grade tumor as in Fig. 3.
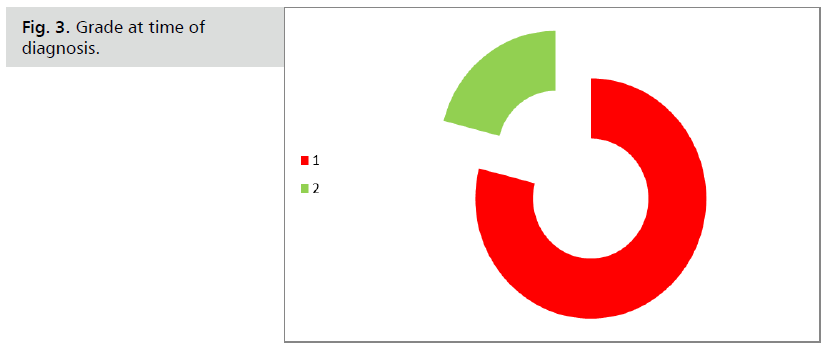
Fig. 3. Grade at time of diagnosis.
The study found that, high percentage of cases about 29 (46.8%) of cases were at stage 2 tumor at time of diagnosis, then stage 1 about 19 (30.6%) then stage 3 14 (22.6%) Fig. 4.
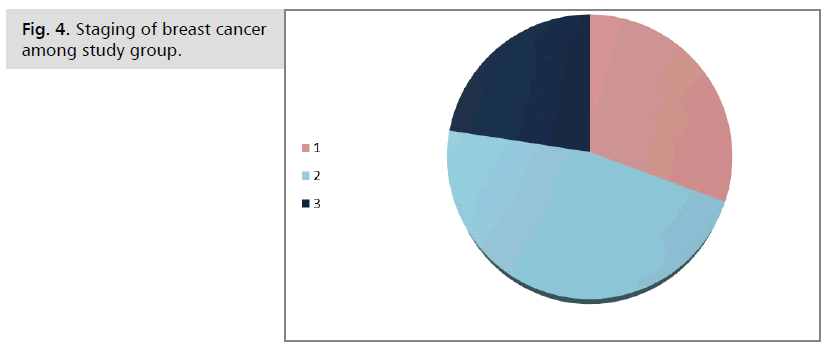
Fig. 4. Staging of breast cancer among study group.
Regarding estrogen receptors, the results proved that 42(67.7%) of cases had negative estrogen receptor while 20 (32.3%) were positive Fig. 5.
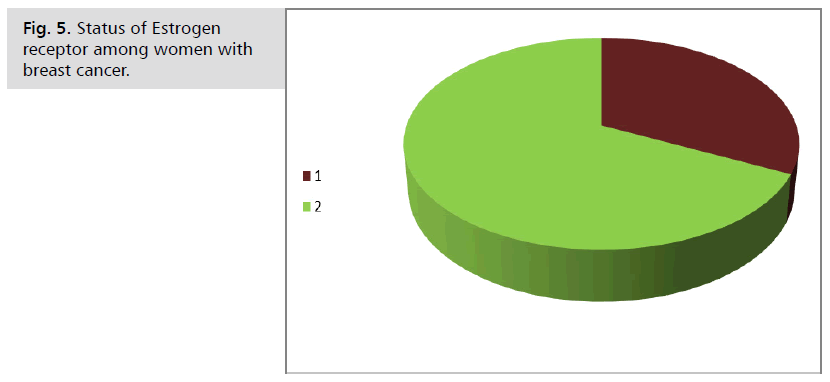
Fig. 5. Status of Estrogen receptor among women with breast cancer.
The current study found that most frequent histopathological type among 55 (88.7%) was ductal carcinoma while 7 (11.3%) cases had lobular type Fig. 6.
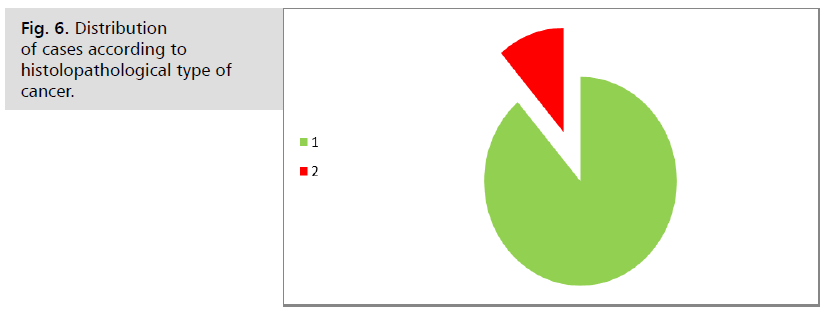
Fig. 6. Distribution of cases according to histolopathological type of cancer.
This study found that, 56(90.3%) of cases had modified radical mastectomy with axillary lymph node dissection. From 62 cases there were only 11 (17.7%) of cases received Neoadjuvant chemotherapy before surgery.
High percent of cases about 38 (86.4%) received chemotherapy after childbirth.
Regarding outcome of cases during year of follow up, there is one case died while other 61 cases still on treatment. Tab. 2.
| Type of management | No. | % | |
|---|---|---|---|
| Surgical procedure | Modified radical mastectomy with axillary lymph node dissection | 56 | 90.3 |
| Conservative surgery plus local radiotherapy | 6 | 9.7 | |
| Neoadjuvant chemotherapy before surgery | Yes | 11 | 17.7 |
| No | 51 | 82.3 | |
| Chemotherapy | Given after childbirth | 38 | 86.4 |
| Before delivery | 6 | 13.6 | |
| Outcome (During first year) | Still on treatment schedule | 61 | 98.4 |
| Death | 1 | 1.6 |
Tab. 2. Fate of breast cancer women in study group.
Discussion
Basically, pregnancy relevant breast cancer and that affecting young girls are rare, but both of them is growing in incidence. Similarly, as the mother age increases, rising numbers of ladies are named to have breast ca just before completing their family members.
Decisions for the management accomplished by a professional team precisely include two persons: the pregnant lady and her newborn. The decision is made by a multidisciplinary but still the surgical role is the cornerstone of the process, The earlier the diagnosis and administration of effective therapy, the best the prognosis for the woman. The more secure choices for the baby are surgical interferences done at any trimester of conception and after child delivery, but some authors prefer to perform any surgical operation to the pregnant ladies during the 2nd trimester if feasible [17]. Chemotherapy is permitted during the (2nd and 3rd) trimesters of conception. The effective and safe medications better be preferred, mainly taxanes or anthracyclines [18]. Radiotherapy in pregnancy is still a source of debate, but due to its crucial role and absence of substitutes, it must be kept into account. It is necessary to outline the correct dosage affecting the fetus to reduce the danger of newborn defects. More recent techniques scheduled for patients with breast carcinoma BC, which involve: hormonal therapy, immunotherapy, are contraindicated in pregnant women. Induced abortion is never indicated [19].
This paper describes the primary definitions of patients with conception-related ca breast and eventual pregnancy. Ladies wishing to have a baby after surviving PABC seemed to be younger and were less likely to deliver kids prior to ca breast diagnoses in comparison with these who didn’t keen on multiple pregnancies.
Several works have shown the safety of oncologic pregnant case after ca breast management. It has been seen in the positive group, women with stage (1-3) hormone receptorpositive ca breast who wanted pregnancy intermittent endocrine medication after 18–30 months from therapy.
Our numbers go with past results in some breast cancer in pregnancy cohorts, which record similar ratios of PR- and ER- Negative lesions in PABC cases between (50-60) percent [12].
Nevertheless, a study from Norway declared that nursing PABC females have a worse prognosis, which may point to a serious disorder with prolactin plasma concentration. A limitation of this thesis is that information was taken from histopathology records, which often doesn’t include clinical data, i.e. stage, imaging results, mother treatment.
A second drawback is the lacking data, i.e. for HER2-Receptor condition in the PABC cohort. The explanation is that by the year 2000, routine HER2-testing was introduced.
An interesting observation, that most of our PABC cases were pregnant ladies, which is in contrary to a previous literature, saying that up to two thirds of diagnosed patients were within twelve months after delivery (postpartum).
To ensure the oncologic safety of pregnancies harboring breast cancer and completed their management plan, an extended metaanalysis involved more than 7500 ladies who were pregnant just after been discovered to have breast carcinoma. Ultimately many of these pregnancies gave result to live births. Yet, in comparison with the general people, there was both a more percentage of cesarean section for these ladies, besides an increased rate of premature babies, low weight births, and small for date newborns to these females treated for ca breast [5].
In another separate meta-analysis from about 16 papers, the percentage of pregnancy among cases with a previous history of ca breast were, nearly, 40% less if compared with the general people, and among those who had been pregnant, the mean range of pregnancy loss by prematurity or miscarriage was 12%. Our findings revealed a comparable rate of pregnancy loss after PABC management; but, the information about mode of delivery and weight of newborns were not reported in our study as many ladies delivered outside our institutions, from which we obtained our data [8].
Nonetheless, focused counseling and further psychosocial rehabilitation are required for this specific society, with a special care for these challenges.
Conclusion
Pregnancy relevant breast carcinoma is uncommon disease entity in Iraq. Its approach and management is comparable to the usual non-pregnant women, but to keep in consideration the essence of treatment vs. the hazards towards both the mother and her baby.
Unfortunately, this topic is neglected, and it demands further researches to figure out the tumor earlier and to improve the quality of care.
References
- Guidroz JA, Scott-Conner CEH, Weigel RJ, et al. Management of pregnant women with breast cancer. J Surg Oncol. 2011;103:337-340.
- Galati F, Magri V, Arias-Cadena P, et al. Pregnancy-associated breast cancer: a diagnostic and therapeutic challenge. Diagnostics. 2023;13:604.
- Heimovaara JH, Boere IA, de Haan J, et al. Ten-year experience of a national multidisciplinary tumour board for cancer and pregnancy in the Netherlands. Eur J Cancer. 2022;171:13-21.
- Azim HA, Santoro L, Russell-Edu W, et al. Prognosis of pregnancy-associated breast cancer: a meta-analysis of 30 studies. Cancer Treat Rev. 2012;38:834-842.
- Cordeiro CN, Gemignani ML, et al. Breast cancer in pregnancy: avoiding fetal harm when maternal treatment is necessary. Breast J. 2017;23:200-205.
- Hartman EK, Eslick GD, et al. The prognosis of women diagnosed with breast cancer before, during and after pregnancy: a meta-analysis. Breast Cancer Res Treat. 2016;160:347-360.
- Sultan Awni I, Habash M, et al. Is breast conserving surgery a suitable approach for early breast carcinoma? A multicenter study. Pak J Med Health Sci. 2022;16:619-622.
- Roesch E, Maggiotto A, Valente SA, et al. Multidisciplinary management of pregnancy-associated breast cancer. JCO Oncol Pract. 2024.
- Soto-Trujillo D, Santos Aragón LN, Kimura Y, et al. Pregnancy-associated breast cancer: what radiologists must know. Cureus. 2020;12:e.
- Kesireddy M, Krishnamurthy J, et al. Pregnancy-associated breast cancer: key concepts for optimizing diagnosis and treatment. Am Soc Clin Oncol. 2024:196-224.
- Amin B, Edge SB, Greene F, et al. American Joint Committee on Cancer (AJCC) cancer staging manual. Eighth edition. New York: Springer. 2017.
- Jo H, Park S, Kim HR, et al. Long-term breast cancer outcomes of pregnancy-associated breast cancer (PABC) in a prospective cohort. Cancers (Basel). 2022;14:4839.
- Zagouri F, Sergentanis TN, Chrysikos D, et al. Trastuzumab administration during pregnancy: a systematic review and meta-analysis. Breast Cancer Res Treat. 2013;137:349-357.
- Partridge AH, Niman SM, Ruggeri M, et al. Interrupting endocrine therapy to attempt pregnancy after breast cancer. N Engl J Med. 2023;388:1645-1656.
- Han SN, Amant F, Cardonick EH, et al. Axillary staging for breast cancer during pregnancy: feasibility and safety of sentinel lymph node biopsy. Breast Cancer Res Treat. 2018;168:551-557.
- Michalet M, Dejean C, Schick U, et al. Radiotherapy and pregnancy. Cancer Radiother. 2022;26:417-423.
- Sultan AI, Habash M, Ghareeb OA, et al. Outcomes of symptomatic gallstone disease in pregnant women: a retrospective study. EJPMR. 2024;11:651-655.
- Framarino-dei-Malatesta M, Piccioni M, Brunelli R, et al. Breast cancer during pregnancy: a retrospective study on obstetrical problems and survival. Eur J Obstet Gynecol Reprod Biol. 2014;173:48-52.
- Ferrigno Guajardo AS, Vaca-Cartagena BF, Mayer EL, et al. Taxanes for the treatment of breast cancer during pregnancy: an international cohort study. J Natl Cancer Inst. 2024;116:239-248.
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Author Info
Basma Hameed Mageed1, Jamal Mohammed Ibrahim2, Awni Ismail Sultan3* and Nisreen Mohammed Ibraheem42Department of Surgery, College of Dentistry, Al Kitab University, Kirkuk, Iraq
3Department of Surgery, College of Medicine, Tikrit University, Tikrit, Iraq
4Department of Community Medicine, College of Medicine, Tikrit University, Tikrit, Iraq
Copyright:This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.