Research - (2022) Volume 17, Issue 4
Predictive value of day 4 β-hCG level after Methotrexate therapy in ectopic pregnancy: A retrospective study
Ahmed Alanwar1*, Waleed M Khalaf1, Marwa A Salem2 and Ibrahim Ali1,3Received: 01-Dec-2022, Manuscript No. gpmp-22-81993; Editor assigned: 02-Dec-2022, Pre QC No. P-81993; Reviewed: 14-Dec-2022, QC No. Q-81993; Revised: 20-Dec-2022, Manuscript No. R-81993; Published: 29-Dec-2022
Abstract
Objectives: To assess the changes in serum beta-human chorionic gonadotrophin (β-hCG) between days 0 and 4 to predict the outcome of methotrexate therapy in ectopic pregnancy.
Methodology: Retrospective descriptive research was performed at the Armed Forces Hospitals of the Southern Region's obstetrics and gynecology department, KSA. Analysis of day 4 β-hCG levels in 198 patients diagnosed with an ectopic pregnancy and treated with a single intramuscular dose of methotrexate (50 mg/m2) from January 2015 till January 2020.
Results: Day 4 serum β-hCG dropped in 120 patients (60.6% of cases), and the success of treatment was achieved in 88.3% of these cases without any further management. Day 4 β-hCG increased in 78 patients (39.4% of cases), only 47.4% of these cases had a success of treatment.
Conclusion: The drop of day 4 serum β-hCG after methotrexate therapy of ectopic pregnancy is a good predictor of treatment success.
Keywords
Methotrexate; Human chorionic gonadotrophin; Ectopic pregnancy.
Introduction
In the past, ectopic pregnancy was managed surgically. In 1989, medical management of ectopic pregnancy in hemodynamically stable patients using single-dose methotrexate was stated safe and acceptable [1,2] with success rates 65-95% [3,4].
In this regimen, a decrease in β-hCG levels of more than 15% between days 4 and 7 after methotrexate administration is considered a successful treatment. Previous researchers have validated this 15% decrease from days 4-7 rule as an excellent predictor of treatment progress, with recorded positive predictive values as high as 93% [5].
The 15 percent reduction rule's potential drawbacks include the following: while waiting for day 7 β-hCG levels, there is a need for patient compliance, the risk of treatment failure, and the risk of ectopic pregnancy rupture [6] unfortunately, no feedback about treatment response can be obtained before day [7]. The presence of an earlier marker of treatment success may give an earlier reassurance [7]. It may have a direct effect on clinical decision-making in some cases, where opting out of medical management and proceeding to surgery is being considered.
According to some researchers [6,7] women whose serum β-hCG dropped between days 0 and 4 after a single dose of methotrexate for an ectopic pregnancy had a remarkable treatment success rate, with no need for further treatment. Those whose serum β-hCG levels increased between days 0 and 4 had a 58 percent risk of failing treatment [7]. These studies gave early prognostic marker without adding any extra tests which could be of good benefit for patients and physicians.
However, the Nguyen et al., [6] and Skubisz et al., [7] studies were small retrospective studies. As a result, independent confirmation is needed before clinicians can consider using serum β-hCG patterns between days 0 and 4 as an early prognostic indicator. As a consequence, we looked at the trend of serum β-hCG levels between day 0 and day 4 and their impact on the success and failure rates of methotrexate therapy for ectopic pregnancies in patients treated at our tertiary hospital over 5 years.
Patients and Methods
Retrospective descriptive research was performed at the Armed Forces Hospitals of the Southern Region's obstetrics and gynecology department, KSA. Approval of the research ethics committee was taken before starting the study. Data were collected from the electronic and hard copy files of women who had been diagnosed with an ectopic pregnancy and treated with a single intramuscular dose of methotrexate (50 mg/m2) from January 2015 till January 2020.
The diagnosis of ectopic pregnancy was made when patients had β-hCG levels above the discrimination zone (1500-2000 IU/L) with the absence of an intrauterine pregnancy by TV US (transvaginal ultrasound) or abnormally rising/ plateauing β-hCG titers below the discrimination zone that is associated with TV US findings that are suggestive of ectopic pregnancy (adnexal mass and/or free fluid in the peritoneal cavity).
Inclusion criteria for the study were hemodynamic stable women, starting β-hCG less than 10000 IU/L, adnexal mass less than 3.5 cm, and complete medical records. Exclusion criteria were hepatorenal dysfunction, abnormal CBC results (WBCs less than 4000 or platelets less than 100000), positive extrauterine cardiac activity, and women with incomplete follow-up or not adherent to the treatment protocol.
The following information was recorded: age, BMI, obstetric and gynecologic history, TV US findings, laboratory values before and after methotrexate therapy, and β-hCG levels on days 0, 4, and 7. In terms of treatment success or failure, the patients were divided into two groups.
After a single dose of methotrexate, treatment success was described as a > 15% decrease in β-hCG levels between days 4 and 7, followed by weekly β-hCG level measurement until negative. The need for a second dose of methotrexate and/or surgery was described as treatment failure. This definition of failure of treatment is the same one used by Nguyen et al., [6] and Skubisz et al., [7].
Statistical analysis was performed using SPSS version 22 for IBM. Description of data was done in form of mean ± SD or median and range for continuous data and number and percentage for categorical data with the Fisher’s exact test for categorical variables and with t-test or Mann-Whitney U test (where appropriate) for continuous variables. ROC receiver operating characteristic curve for detection of best cutoff value with highest sensitivity and specificity. A value of ≤0 .05 was considered statistically significant.
Results
279 cases were managed with single-dose methotrexate due to non-disturbed ectopic pregnancy at the hospital from January 2015 to January 2020. After applying the inclusion and exclusion criteria, only 198 patients were enrolled in that study.
There was no significant difference between treatment failure or success groups after a single dose of methotrexate as regards demographic data (Tab. 1.). The overall rate of treatment success was 72.2 % (143/198 cases). In 60.6% of cases (120/198), β-hCG levels fell between days 0 and 4; in 39.4% of cases (78/198), β-hCG levels rose between days 0 and 4. Treatment success was achieved in 88.3 percent of patients (106/120) who had decreased β-hCG levels between days 0 and 4. In the community where β-hCG levels increased between days 0 and 4, only 47.4 percent of the patients (37/78) had treatment success (Tab. 2.).
| Variables | Treatment success | Treatment failure | P value |
|---|---|---|---|
| Age (years) | 32.66 ± 5.61 | 31.25 ± 6.63 | 0.136 |
| BMI | 27.53 ± 4.2 | 26.43 ± 5.23 | 0.155 |
| Parity | 2.64 ± 2.11 | 2.3 ± 1.95 | 0.314 |
| Ectopic size (mm) | 17.2 ± 7.63 | 17.71 ± 13.73 | 0.750 |
| Pelvic collection (ml) | 44.89 ± 44 | 45.56 ± 45.15 | 0.961 |
Tab. 1. Descriptive data of studied groups.
| HCG change | Success of treatment | Failure of treatment | Total | X² | P |
|---|---|---|---|---|---|
| Decreased | 106(88.3%) | 14(11.7%) | 120(60.6%) | 39.4 | <0.001 |
| Increased | 37(47.4%) | 41(52.6%) | 78(39.4%) | ||
| Total | 143(72.2%) | 55(27.8%) | 198 |
Tab. 2. hCG change from day 0 to day 4 and relation with successes of treatment.
The output of β-hCG difference between day 0 and day 4 in both groups of treatment success and failure was assessed using the receiver operator curve (ROC) (Fig. 1. and Tab. 3.). According to the ROC, a 20 percent decrease in β-hCG between days 0 and 4 had a sensitivity of 0.5, specificity of 0.89, positive predictive value of 0.82, and negative predictive value of 0.64. That is, 89% of cases who experienced treatment failure had a decrease in β-hCG difference less than 20%, and if β-hCG difference decreased more than 20%, it can predict treatment success in 82% of cases after a single dose of methotrexate (Tab. 4.)
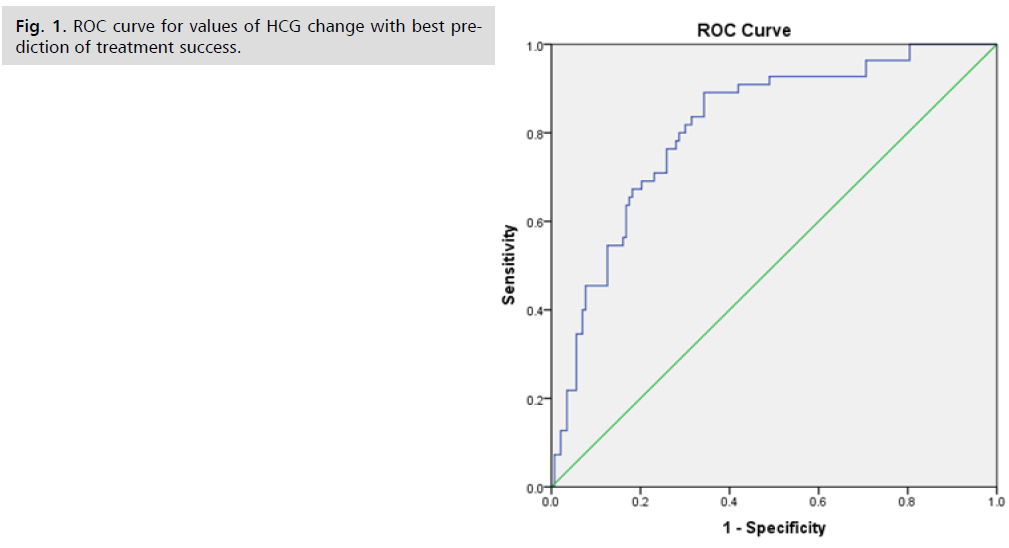
Fig 1. ROC curve for values of HCG change with best prediction of treatment success.
| Asymptotic 95% Confidence Interval | ||||
|---|---|---|---|---|
| Area | Standard Errora | Asymptotic Significanceb | Lower Bound | Upper Bound |
| 0.813 | 0.033 | 0.000 | 0.749 | 0.878 |
bNull hypothesis: true area = 0.5
Tab. 3. ROC curve for values of HCG change.
| Variables | Decreased 20% | Increased 20% |
|---|---|---|
| Sensitivity | 0.50 [0.40, 0.60] | 0.50 [0.40, 0.60] |
| Specificity | 0.89 [0.81, 0.94] | 0.92 [0.84, 0.96] |
| Positive predictive value | 0.82 [0.70, 0.90] | 0.86 [0.74, 0.93] |
| Negative predictive value | 0.64 [0.55, 0.72] | 0.65 [0.56, 0.72] |
Tab. 4. β-hCG difference between day 0 and day 4 and prediction of treatment success and failure.
The ROC detected that β-hCG difference of 20% increase between day 0 and day 4 had sensitivity 0.5, specificity 0.92, positive predictive value 0.86, and negative predictive value 0.65. That is, 92% of cases who experienced treatment success had an increase in β-hCG difference of less than 20%, and if β-hCG difference increased more than 20%, it can predict treatment failure in 86% of cases after a single-dose of methotrexate. (Tab. 4.)
Discussion
The best predictor of single dose methotrexate therapy efficacy for ectopic pregnancy management is currently unknown. High β-hCG concentrations (5000 IU/mL), fetal cardiac activity, greater ectopic size (4 cm), and sonographic evidence of free peritoneal fluid are all known predictors of methotrexate treatment failure [8]. The increase in β-hCG in the 48 hours leading up to treatment has also been proposed as a new predictor of methotrexate effectiveness, with smaller increments indicating a higher chance of success [9].
Early β-hCG changes after single-dose methotrexate for ectopic pregnancy could predict the likelihood of therapy outcome, according to this retrospective study. It was discovered that a decline was linked to an 88.3 percent chance of success without the need for additional methotrexate or surgery. Those who had a rise, on the other hand, just had a 47.4 percent chance of successful treatment. As a result, a decrease in serum β-hCG by day 4 after methotrexate appears to be reassuring, whereas an increase in serum β-hCG appears to be less so.
Skubisz et al., [7] findings are widely supported by our research, who found that 88 percent of patients (29/33) who had a decrease in serum β-hCG between days 0 and 4 had treatment success in a 45-cases study. Although our success rate was not as high as that recorded by Nguyen et al.6 in a study of 30 participants, all 12 patients who had a decrease in β-hCG between days 0 and 4 had treatment success (100 percent success rate). We still believe that an early drop in serum β-hCG is correlated with a high likelihood of treatment success.
A study by Agostini et al., [10] backs up the claim that a decrease in serum β-hCG between days 0 and 4 is a highly reassuring finding, who found that if the rate of β-hCG decline between days 0 and 4 was >20 percent, there was a 97 percent chance of treatment success. However, their definition of clinical success included those that needed several doses of methotrexate, so it is not directly comparable to ours. As a result, it's not surprising that the group with a drop in serum β-hCG of more than 20% has a higher rate of effective treatment.
The risk of failure or the need for a second injection, as well as patient compliance, is two major issues that should be considered after a methotrexate injection [10]. There is no way to tell whether methotrexate is functioning until at least day 7 with current protocols. A predictive test that provides an early indicator of possible treatment outcomes by day 4 is clinically useful. It can give early reassurance to anxious patients who are waiting for a potentially life-threatening condition to be resolved [7]. So, the cases with β-hCG difference of more than 20% drop on day 4 may not be offered a follow up on day 7 and offered fewer numbers follow up visits after methotrexate therapy (the chance of success is 82 percent), This could save them from getting a second dose of methotrexate that they don't need, but since the chance of success is not 100%, follow up is still needed for these patients. In contrast, the cases with β-hCG difference of more than 20% rise on day 4 may be offered a second dose of methotrexate earlier than day 7 (the chance of failure is 86%) which could theoretically improve medical management success rates and/or shorten the time it takes for ectopic pregnancies to resolve.
Conclusion
The early β-hCG level changes after methotrexate therapy for ectopic pregnancy have a variety of applications. When a more resistant disease is detected early, it can be treated more vigorously. On the other hand, Patients with early β-hCG level changes that indicate treatment success may need less follow-up evaluation. Furthermore, when a patient is counseled about treatment choices and her prognosis, this knowledge can be useful.
Authors Contribution
(A) Study Design · (B) Data Collection · (C) Statistical Analysis · (D) Data Interpretation · (E) Manuscript Preparation · (F) Literature Search · (G) No Fund Collection
References
- Stovall TG, Ling FW, Buster JE. Outpatient chemotherapy of unruptured ectopic pregnancy. Fertil Steril. 1989;51(3):435-438.
- Stovall TG, Ling FW, Gray LA. Single-dose methotrexate for treatment of ectopic pregnancy. Obstet Gynecol. 1991;77(5):754-757.
- Stovall TG, Ling FW. Single-dose methotrexate: an expanded clinical trial. Am J Obstet Gynecol. 1993;168(6):1759-1765.
- Bixby S, Tello R, Kuligowska E. Presence of a yolk sac on transvaginal sonography is the most reliable predictor of single‐dose methotrexate treatment failure in ectopic pregnancy. J Med Ultrasound. 2005;24(5):591-598.
- Kirk E, Condous G, Van Calster B, et al. A validation of the most commonly used protocol to predict the success of single-dose methotrexate in the treatment of ectopic pregnancy. Hum Reprod. 2007;22(3):858-863.
- Nguyen Q, Kapitz M, Downes K, et al. Are early human chorionic gonadotropin levels after methotrexate therapy a predictor of response in ectopic pregnancy?. Am J Obstet Gynecol 2010;202(6):630-e1.
- Skubisz MM, Lee J, Wallace EM, Tong S. Decline in βhCG levels between days 0 and 4 after a single dose of methotrexate for ectopic pregnancy predicts treatment success: a retrospective cohort study. BJOG. 2011;118(13):1665-1668.
- Practice Committee of the American Society for Reproductive Medicine. Medical treatment of ectopic pregnancy. Fertil Steril. 2008;90(5):S206-S212.
- da Costa Soares R, Junior JE, Camano L. Increment in β-hCG in the 48-h period prior to treatment: A new variable predictive of therapeutic success in the treatment of ectopic pregnancy with methotrexate. Arch Gynecol Obstet. 2008;278(4):319-324.
- Agostini A, Blanc K, Ronda I, et al. Prognostic value of human chorionic gonadotropin changes after methotrexate injection for ectopic pregnancy. Fertil Steril. 2007;88(2):504-506.
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Author Info
Ahmed Alanwar1*, Waleed M Khalaf1, Marwa A Salem2 and Ibrahim Ali1,32King Faisal Military hospital (Imam Abdulrahman Bin Faisal hospital), NGH, Dammam, Saudi Arabia
3King Faisal Military hospital (Armed forces Hospitals), Southern Region, Saudi Arabia
Copyright:This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.