Research - (2025) Volume 20, Issue 3
Investigation of the effect of uterosacral ligament plication ñn preventing cuff prolapse
Belma Gözde Özdemir1*, Meltem Aydoğdu3, Betül Dik1, Leyla Huseynli1, Günay Safarova1, Ahmet Bilgi1, Mustafa Gazi Uçar1 and Çetin Çelik1Received: 20-Jun-2025, Manuscript No. gpmp-25-167764; Editor assigned: 23-Jun-2025, Pre QC No. P-167764; Reviewed: 15-Jul-2025, QC No. Q-167764; Revised: 23-Jul-2025 Published: 29-Aug-2025
Abstract
Background/Aim: Following a hysterectomy, the incidence of cuff prolapse is 3.2%, whereas among women who have not undergone a hysterectomy, the prevalence is 2%. This difference is significant, as the uterine ligaments play a crucial role in maintaining the uterus's position. The ligament structure is disrupted by the aging process, which also affects the extracellular matrix and metalloproteinase activity. However, anatomic loss of support structure happens following a hysterectomy. Apical prolapse and subsequent scar tissue may be avoided by stabilizing sutures to the uterosacral ligament's cuff. Apical prolapse and subsequent scar tissue may be avoided by stabilizing sutures to the uterosacral ligament's cuff. This study aims to investigate the effectiveness of Uterosacral Ligament Plication (USLP) in preventing cuff prolapse after hysterectomy. Material/Methods: A retrospective study was conducted, evaluating all cases that underwent total abdominal hysterectomy for benign or malignant reasons between 2010 and 2024. Among these, patients who developed cuff prolapse and underwent surgery for this reason were identified. Patients who underwent USLP and those who did not were categorized. A total of 2033 patients underwent hysterectomy; 832 underwent USLP, and the cuff was closed with continuous locking in 1201 patients. Results: According to these data, there was a statistically significant difference in the rates of vaginal cuff prolapse between the two groups (p<0.05). The incidence of cuff prolapse is higher when the USLP technique is not added. Conclusion: Applying USLP to close the vaginal cuff, which is an easy and applicable method, may be a preventive step against cuff prolapse.
References
Blog | Real Estate in Belgium Security Technologies Articles Blog | Real Estate in Portugal Technology Equipment Articles Blog | Real Estate in Canada Tools Technologies Articles Blog | Casino Sites in Sweden Blog | Mortgage info in California Video Technologies Articles Blog | Real Estate in Cambodia Aesthetics Surgical Articles of Cancer Blog | Where Buy NFT's Blog | Mortgage info in Oklahoma Blog | Casino Sites in Spain Cos Surgery Journals Blog | Car Insurance in Oklahoma Ent Articles Epilepsy Journals Eye Surgery JournalsKeywords
Cuff prolapse; Hysterectomy; Uterosacral ligament; Technical procedure
Introduction
Hysterectomy is the most frequently performed gynecological surgery worldwide for both benign and malignant reasons. Despite advances in surgical techniques, apical or vaginal cuff prolapse, in particular, remains a significant long-term complication after hysterectomy. While the prevalence of apical prolapse is approximately 2% in women who have not undergone hysterectomy, this rate is reported to increase to 3.2% after hysterectomy. This highlights the role of anatomical structures supporting the uterus in pelvic floor support [1].
Literature has shown that hysterectomy is an independent risk factor for the development of pelvic organ prolapse. In an extensive national cohort study by Husby, et al., nulliparous women who underwent hysterectomy for benign indications were found to have approximately a 60% increased risk of pelvic organ prolapse, regardless of the surgical approach [2]. These findings suggest that surgical disruption of ligamentous support structures, rather than obstetric history, plays a primary role in the development of prolapse.
The etiology of vaginal cuff prolapse is likely multifactorial. Age-related weakening of pelvic connective tissue, collagen and elastin loss, changes in extracellular matrix metabolism, and a hypoestrogenic environment negatively affect the loss of pelvic support structures. Furthermore, a history of previous pelvic surgery, delayed wound healing, the presence of preoperative pelvic organ prolapse, and surgical scar tissue formation are essential factors that increase the risk of apical prolapse after hysterectomy [3, 4]. Therefore, conservative surgical approaches aimed at preserving or restoring apical support during hysterectomy are becoming increasingly important. Preventing its formation will reduce subsequent surgical burdens. One of the most important anatomical structures in providing apical support is the uterosacral ligament. Uterosacral ligament suspension or plication is a prophylactic technique aimed at restoring level I support by fixing the vaginal cuff to these ligaments. The amount of plication to be performed is determined according to the atrophic status of the ligament and the mobility of the vaginal cuff [5]. Uterosacral ligament plication is a method that can be performed both abdominally and vaginally, and its effectiveness and safety have been demonstrated in the literatüre [6]. This study aims to investigate the efficacy of uterosacral ligament plication in preventing cuff prolapse after hysterectomy.
Material and Methods
Study design and patient population
This is a retrospective observational study evaluating patients who underwent Total Abdominal Hysterectomy (TAH) for benign or malignant indications at the Department of Obstetrics and Gynecology, Selçuk University Faculty of Medicine, between 2010 and 2024. Medical records of all patients included in the study were reviewed through the hospital archive system. Patients who developed vaginal cuff prolapse after hysterectomy and therefore required surgical treatment were identified. Patients were divided into two groups based on whether or not Uterosacral Ligament Plication (USLP) was performed during vaginal cuff closure. Patients who underwent USLP were defined as the USLP group, while those who underwent vaginal cuff closure using the classical technique were defined as the non-USLP group. Age, comorbidities, gravity, parity, previous surgery, indication for total abdominal hysterectomy, final pathology results, and history of chemotherapy and radiotherapy for exclusion were all investigated. The degree of pelvic organ prolapse and the POP-Q classification are also used [7].
Group 1: USLP not performed = 59.1% (n=1201)
Group 2: USLP performed = 40.9% (n=832)
Inclusion and exclusion criteria
Patients with no prior history of pelvic organ prolapse or surgery due to prolapse, no collagen tissue disease, and who had undergone primary total abdominal hysterectomy were included in the study. Patients diagnosed with pelvic organ prolapse before hysterectomy, those who had undergone previous pelvic floor surgery, and those with incomplete medical records were excluded. Additionally, patients who received pelvic or abdominal radiotherapy, cuff brachytherapy, or chemotherapy were omitted.
Surgical technique
All surgical procedures were performed by experienced gynecologists from the Department of Obstetrics and Gynecology, Selçuk University Faculty of Medicine, using the standard total abdominal hysterectomy technique. In the group without USLP, the vaginal cuff was closed using the continuous locking suture technique with the classical method. In the group that underwent USLP, No. 1 polyglactin (Vicryl®) sutures were placed sequentially at the corners of the vaginal cuff. These sutures were secured bilaterally to the uterosacral ligaments to achieve plication, after which the vaginal cuff was closed entirely. The amount of plication performed was determined by the surgeon according to the atrophic status of the uterosacral ligament and the mobility of the vaginal cuff (Fig. 1.). Both uterosacral ligaments are symmetrically harvested to the posterior cervix or the apex of the vaginal vault using non-absorbable or slow-absorbable sutures of size 0 or 1, and ligated by bringing them closer together towards the midline, thus shortening the ligaments and increasing apical support; avoiding suturing too laterally and holding the ligament at a sufficiently strong point reduces the risk of ureteral injury and suture rupture. Abdominal uterosacral ligament plication is considered an advantageous method because it can provide results consistent with the anatomical axis [8-10].
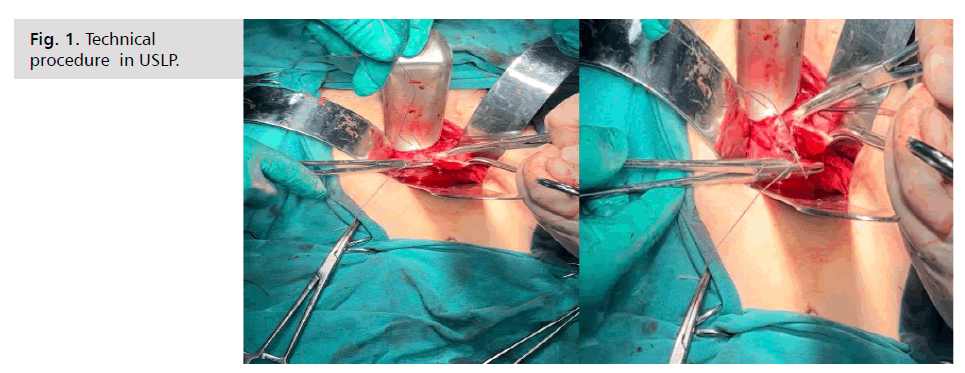
Fig. 1. Technical procedure in USLP.
Data collection and variables
The demographic characteristics of the patients (age, sociodemographic data), surgical indications, surgical technique used, USLP application status, and whether vaginal cuff prolapse developed in the postoperative period were recorded. Vaginal cuff prolapse was diagnosed using clinical examination and the Pelvic Organ Prolapse (POP-Q) system. Patients requiring surgical intervention due to prolapse were also noted.
Ethical number: Approval has been obtained from the Selçuk University Ethics Committee. E-70632468-050.04-922353
Statistical Analysis
Statistical analysis of the data was performed using the Statistical Package for the Social Sciences (SPSS) version 26.0. Data on the technical performance of the hysterectomy and the occurrence of vaginal cuff prolapse were presented as counts and percentages. The Chi-square test was used to evaluate the relationship between the surgeon who performed the hysterectomy and the development of vaginal cuff prolapse. Statistical significance levels were accepted as 0.05 and 0.01 for the entire study.
Results
A total of 2033 patients were included in the study. The mean age of the patients was 52.4 ± 3.2 years. When evaluating comorbidities, diabetes mellitus and hypertension were the most frequently observed. Regarding previous surgical history, cesarean section was the most common operation. The vast majority of patients were multiparous. When surgical indications were examined, 65% (n=1321) of patients underwent surgery for benign causes, and 35% (n=712) for malignant causes. Final pathology results confirmed malignancy diagnoses. No statistically significant difference was found between the groups that underwent USLP and those that did not regarding surgical indications (p>0.05).
Of the patients who underwent hysterectomy, 59.1% (n=1201) did not undergo uterosacral ligament plication (USLP), whereas 40.9% (n=832) did. When vaginal cuff prolapse was evaluated, it was observed that 99.2% (n=2016) of patients did not develop prolapse, while 0.8% (n=17) had prolapse. All patients operated on due to prolapse were evaluated as having total vaginal cuff prolapse. In 27% (n=5/17) of these patients, in addition to total cuff prolapse, anterior and posterior compartment prolapse was also observed (Tab. 1.).
| USLP Status | Cuff Prolapse Present n (%) | Cuff Prolapse Absent n (%) | Total n (%) | p value |
|---|---|---|---|---|
| USLP performed | 2 (0.2%) | 830 (99.8%) | 832 (100) | - |
| USLP not performed | 15 (1.2%) | 1186 (98.8%) | 1201 (100) | - |
| Total | 17 (0.8%) | 2016 (99.2%) | 2033 (100) | 0.027* |
Tab. 1. . Distribution of vaginal cuff prolapse according to Uterosacral Ligament Plication (USLP).
In 99.8% (n=830/832) of patients who underwent USLP during hysterectomy, vaginal cuff prolapse was not observed, while it developed in only 0.2% (2/832). In the group that did not undergo USLP, prolapse was not observed in 98.8% (n=1186/1201) of patients, while it was detected in 1.2% (15/1201). When both groups were compared, a statistically significant difference was found in the rates of vaginal cuff prolapse (p<0.05). The incidence of vaginal cuff prolapse was observed to be higher in cases where the USLP technique was not applied.
Discussion
This retrospective study demonstrated that uterosacral ligament plication performed during total abdominal hysterectomy significantly reduced the incidence of vaginal cuff prolapse compared to classic vaginal cuff closure techniques.
In this study, no statistically significant difference was found between the groups that underwent and did not undergo USLP in terms of demographic characteristics (age, parity, comorbidities, and surgical indications). However, there was also no significant difference between the groups with respect to known risk factors for pelvic organ prolapse in the literature, such as advanced age, multiparity, history of pelvic surgery, weak connective tissue, and concomitant systemic diseases. This suggests that the significant difference in vaginal cuff prolapse incidence in our study is related to the surgical technique of uterosacral ligament plication rather than patient characteristics [11].
In long-term follow-up studies by Gabriel, et al., it was observed that the risk of developing pelvic organ prolapse after abdominal, laparoscopic, and vaginal hysterectomy persisted regardless of the surgical approach, and the risk of prolapse was significantly increased in cases where apical support was insufficient [12]. These findings reveal that preserving or strengthening apical support structures, as well as the surgical technique used during hysterectomy, are critical. In this study, the significantly higher incidence of vaginal cuff prolapse in patients who did not undergo uterosacral ligament plication during total abdominal hysterectomy supports these results. In particular, compared with this study, which found that the risk of prolapse persisted regardless of the surgical approach, our study did not consider other risk factors, which constitutes a limitation. Adding protective procedures to routine surgical practice may help reduce the long-term risk of prolapse.
In the literature, the modified extraperitoneal uterosacral ligament suspension technique, performed after vaginal hysterectomy, has been reported to be an effective and safe method for preventing vault prolapse [13]. In our study, the significantly higher rates of vaginal cuff prolapse in patients who did not undergo uterosacral ligament plication during total abdominal hysterectomy are consistent with the results of Pal and Bandyopadhyay. Although the study in question included vaginal hysterectomy cases, it is thought that the uterosacral ligament is the primary method for preserving apical support. In this context, it can be said that abdominally performed uterosacral ligament plication is also effective in preventing vaginal vault prolapse.
Lukanovic and Drazic reported that advanced age, multiparity, history of previous pelvic surgery, and weak connective tissue are essential risk determinants for the development of vaginal prolapse after hysterectomy [14]. In their study, they emphasized that the risk of prolapse is significantly increased, especially when apical support is insufficient. In our research, the fact that the majority of patients were multiparous and the most frequent previous surgery was cesarean section is consistent with the risk factors described in the literature. However, despite this high-risk profile, the significantly lower rates of vaginal cuff prolapse in the group that underwent uterosacral ligament plication during total abdominal hysterectomy suggest that USLP may be a protective surgical approach that can balance the adverse effects of these risk factors.
In their study evaluating the need for reoperation due to vaginal vault prolapse after hysterectomy, Dällenbach, et al. stated that inadequate apical support during surgery, in addition to the patient's demographic characteristics, may be a risk factor in the development of prolapse [15]. In our study, although there was no significant difference between the groups that underwent and did not undergo USLP in terms of baseline demographic characteristics and known risk factors for pelvic organ prolapse, the significantly higher rates of vaginal cuff prolapse in patients who did not undergo uterosacral ligament plication support these findings.
In studies evaluating risk factors for pelvic organ prolapse recurrence in patients undergoing vaginal hysterectomy with sacrospinous hysteropexy and uterosacral ligament suspension, the literature indicates that the adequacy of apical support, independent of surgical technique, is one of the most critical factors determining the risk of recurrence [16]. In their studies, they emphasized that prolapse recurrence was more frequent in cases with insufficient apical support, even when patient characteristics and known prolapse risk factors were similar. Our study is consistent with these results. This finding suggests that strengthening apical support during surgery will be effective in reducing patient-related risk factors.
In their study investigating the effect of angle-stitch application during abdominal hysterectomy on the development of vaginal vault prolapse, Rahn, et al. showed that suture techniques that provide additional apical support during hysterectomy reduced the long-term risk of vault prolapse [17]. This study emphasized that simple supports added to the surgery significantly contributed to preserving pelvic floor anatomy. In our research, uterosacral ligament plication during abdominal hysterectomy significantly reduced the incidence of vaginal cuff prolapse compared with the classic vaginal cuff closure technique, consistent with the results of Rahn, et al. with the angle stitch technique. The presence of midline support as a surgical technique is essential in this respect. This similarity also shows alternative schemes of different apical support techniques applied abdominally.
However, studies in the literature also report that the effect of surgical techniques on the development of pelvic organ prolapse is limited [18]. Dietz, et al. reported that patient-related factors such as birth trauma, connective tissue characteristics, and levator ani injury may be more decisive in the etiology of prolapse than surgical interventions. In this study, it was emphasized that surgical techniques that provide additional apical support may not confer a protective effect in all patient groups. This contradicts our findings.
However, there are also studies in the literature reporting limited evidence that prophylactic apical support interventions reduce the long-term risk of pelvic organ prolapse in all patient groups. A Cochrane review by Maher, et al. stated that apical support techniques can improve short-term anatomical outcomes, but long-term outcomes are significantly affected by patient-related factors [19]. This review concluded that a higher level of evidence is needed for the routine use of prophylactic apical support. In contrast, our study found it effective in the long term, based on the patients' long-term follow-up.
Interestingly, another study in the literature suggests that anatomical restoration does not have the expected high impact. Barber, et al. have shown that there is not always a direct relationship between anatomical restoration and long-term clinical success and patient satisfaction in prolapse surgery [20]. This study emphasizes that additional supportive surgical techniques may have a limited effect on the development of prolapse in some patient groups. It is understood that individual risk factors and extra characteristics are essential for evaluation.
Study Limitations
This study has some limitations. First, the single-center, retrospective design of the study may limit the generalizability of the results. Additionally, some cases could not be included in the study due to the disorganized or incomplete medical records of patients who were not operated on at the exact center. The fact that the POP-Q classification for vaginal cuff prolapse was performed based on patient records may have led to relatively subjective results compared to a prospective assessment based on clinical examination. For these reasons, the findings need to be supported by multicenter and prospective studies in larger patient groups.
In conclusion, uterosacral ligament plication stands out as an easily applicable, low-morbidity, and effective prophylactic method during total abdominal hysterectomy. It can be performed as part of routine surgical procedures, especially in patients with risk factors, with the expectation of long-term effects.
Conclusion
Evaluating the short-term and long-term outcomes of each surgery separately is an art of surgery. Prevention can be achieved by adding the USLP technique, a practical and easily applicable technique, to the end of the procedure. Patients should be evaluated in detail, especially regarding their quality of life and potential long-term morbidities.
Conflict of Interest
No conflict of interest.
Acknowledgment
All necessary permissions and ethics committee approvals are available.
Complies with Helsinki Decleration rules.
References
- Pedersen KD, Storkholm MH, Bek KM, et al. Recurrent apical prolapse after high uterosacral ligament suspension - in a heterogenous cohort characterised by a high prevalence of previous pelvic operations. BMC Womens Health. 2019;19(1):96.
- Husby KR, Gradel KO, Klarskov N, et al. Pelvic organ prolapse following hysterectomy on benign indication: a nationwide, nulliparous cohort study. Am J Obstet Gynecol. 2022;226(3):386.e1-386.e9.
- Kadiroğulları P, Seckin KD, Akselim B, et al. Modified extraperitoneal uterosacral ligament suspension in preventing cuff prolapse risk after vaginal hysterectomy; 4 clamp method. J Invest Surg. 2020;33(8):723-729.
- Collins S, Lewicky-Gaupp C, Sung VW, et al. Pelvic organ prolapse. Gastroenterol Clin North Am. 2022;51(1):177-193.
- Schulten SFM, Detollenaere RJ, Stekelenburg J, et al. Sacrospinous hysteropexy vs. vaginal hysterectomy with uterosacral ligament suspension in women with uterine prolapse stage 2 or higher: observational follow-up of a multicentre randomised trial. BMJ. 2019;366:l5149.
- Jeppson PC, Sung VW, Muffly TM, et al. Hysterectomy for pelvic organ prolapse: indications and techniques. Clin Obstet Gynecol. 2014;57(1):72-82.
- Persu C, Chapple CR, Cauni V, et al. Pelvic Organ Prolapse Quantification System (POP–Q)–a new era in pelvic prolapse staging. J Med Life. 2011;4(1):75.
- Barber MD, Maher C. Apical prolapse. Int Urogynecol J. 2013;24(11):1815-1833.
- DeLancey JO. Anatomie aspects of vaginal eversion after hysterectomy. Am J Obstet Gynecol. 1992;166(6):1717-1728.
- Prolapse PO. ACOG Practice Bulletin. Obstet Gynecol. 2019;134(5):e126-e142.
- Swift S, Woodman P, O'Boyle A, et al. Pelvic Organ Support Study (POSST): the distribution, clinical definition, and epidemiologic condition of pelvic organ support defects. Am J Obstet Gynecol. 2005;192(3):795-806.
- Gabriel I, Kalousdian A, Brito LG, et al. Pelvic organ prolapse after 3 modes of hysterectomy: long-term follow-up. Am J Obstet Gynecol. 2021;224(5):496.e1-496.e10.
- Pal M, Bandyopadhyay S, Chatterjee G, et al. Modified extraperitoneal uterosacral ligament suspension for prevention of vault prolapse after vaginal hysterectomy. Int Urogynecol J. 2019;30(4):633-637.
- Lukanovic A, Drazic K, But I, et al. Risk factors for vaginal prolapse after hysterectomy. Int J Gynaecol Obstet. 2010;110(1):27-30.
- Dällenbach P, Kaelin-Gambirasio I, Jacob S, et al. Incidence rate and risk factors for vaginal vault prolapse repair after hysterectomy. Int Urogynecol J Pelvic Floor Dysfunct. 2008;19(12):1623-1629.
- Schulten SF, Detollenaere RJ, IntHout J, et al. Risk factors for pelvic organ prolapse recurrence after sacrospinous hysteropexy or vaginal hysterectomy with uterosacral ligament suspension. Am J Obstet Gynecol. 2022;227(2):252.e1-252.e9.
- Rahn DD, Stone RJ, Vu AK, et al. Abdominal hysterectomy with or without angle stitch: correlation with subsequent vaginal vault prolapse. Am J Obstet Gynecol. 2008;199(6):669.e1-669.e4.
- Dietz HP, Steensma AB. The role of childbirth in the aetiology of rectocele. BJOG. 2006;113(3):264-267.
- Maher C, Feiner B, Baessler K, et al. Surgical management of pelvic organ prolapse in women. Cochrane Database Syst Rev. 2013(4).
- Barber MD, Brubaker L, Nygaard I, et al. Defining success after surgery for pelvic organ prolapse. Obstet Gynecol. 2009;114(3):600-609.
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Author Info
Belma Gözde Özdemir1*, Meltem Aydoğdu3, Betül Dik1, Leyla Huseynli1, Günay Safarova1, Ahmet Bilgi1, Mustafa Gazi Uçar1 and Çetin Çelik12Department of Gynecology and Obstetrics, Faculty of Medicine, Yalova University, Yalova, Turkey
3Department Gynecology and Obstetrics, Faculty of Medicine,, Selçuk University, Konya,, Turkey
Copyright:This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.