Research - (2025) Volume 20, Issue 2
Impact of preeclampsia on some left ventricular systolic and diastolic function characteristics
Manal Yahya I. AL-Muhana1* and Amina A B AL Dujeli2Received: 06-Mar-2025, Manuscript No. gpmp-25-163759; Editor assigned: 07-Mar-2025, Pre QC No. P-163759; Reviewed: 28-Mar-2025, QC No. Q-163759; Revised: 04-Apr-2025, Manuscript No. R-163759; Published: 30-Jun-2025
Abstract
Background: Numerous studies have shown that a considerable percentage of women with Preeclampsia (PE) or Gestational Hypertension (GH) have cardiovascular maladaptation. One of the main factors contributing to maternal cardiovascular death and morbidity is preeclampsia. Increases in Peripheral Vascular Resistance (PVR) and Left Ventricular mass (LV mass) can be indicators of poor outcomes for both the mother and the fetus. Echocardiography can identify diastolic dysfunction in preeclamptic women, allowing for early intervention.
Aim: The study's objective is to assess some aspects of the left ventricle's systolic and diastolic performance in preeclamptic pregnant women and contrast them with those of normotensive pregnancies.
Methods: case-control study was conducted at AL-Hussain Medical City between January 2023 and January 2024. Group I [n=30] consisted of pregnant women with preeclampsia, and Group II [n=30] consisted of pregnant women with normotension. The diastolic (E/A and E/Em) and systolic (EF) left ventricular functions of both groups were measured using maternal echocardiography.
Result: There were no statistically significant differences between both groups in systolic function parameter (EF) (p>0.05), nor conventional E/A ratio, whereas there were statistically significant differences in the E/Em ratio (p<0.05).
Conclusion: In mild preeclamptic patients, impaired diastolic functions were observed. This finding suggests that assessment of diastolic function during the early stages of pregnancy may have potential as a predictor of preeclampsia.
References
Biotechnology Article Blog | Auto Insurance in Illinois Computer Technologies Articles Blog | Car Insurance in Washington and Georgia Blog | Cordblood Journals Electronic Technologies Articles Blog | Dental Care Journals Emerging Technologies Articles Blog | Best Betting Sites in Italy Environmental Technologies Articles Blog | Car Insurance in Texas Medical Technologies Articles Blog | Casino Sites in Italy Micro Technologies Articles Blog - Find Lawyer in Oklahoma Military Technologies Articles Blog - Find Lawyer in South Carolina Nano Technologies Articles Blog | Best Betting Sites in Argentina Nft Technologies ArticlesKeywords
Preeclampsia; Diastolic function; Systolic function; Ejection fraction
Abstract
Background: Numerous studies have shown that a considerable percentage of women with Preeclampsia (PE) or Gestational Hypertension (GH) have cardiovascular maladaptation. One of the main factors contributing to maternal cardiovascular death and morbidity is preeclampsia. Increases in Peripheral Vascular Resistance (PVR) and Left Ventricular mass (LV mass) can be indicators of poor outcomes for both the mother and the fetus. Echocardiography can identify diastolic dysfunction in preeclamptic women, allowing for early intervention.
Aim: The study's objective is to assess some aspects of the left ventricle's systolic and diastolic performance in preeclamptic pregnant women and contrast them with those of normotensive pregnancies.
Methods: case-control study was conducted at AL-Hussain Medical City between January 2023 and January 2024. Group I [n=30] consisted of pregnant women with preeclampsia, and Group II [n=30] consisted of pregnant women with normotension. The diastolic (E/A and E/Em) and systolic (EF) left ventricular functions of both groups were measured using maternal echocardiography.
Result: There were no statistically significant differences between both groups in systolic function parameter (EF) (p>0.05), nor conventional E/A ratio, whereas there were statistically significant differences in the E/Em ratio (p<0.05).
Conclusion: In mild preeclamptic patients, impaired diastolic functions were observed. This finding suggests that assessment of diastolic function during the early stages of pregnancy may have potential as a predictor of preeclampsia.
Introduction
Pregnancy's high metabolic demands necessitate certain physiological and anatomical adjustments. Nearly every organ system is impacted by these modifications, including the cardiovascular system. As the pregnancy progresses, these physiological adjustments take place to meet the needs of the developing fetus and mother. The majority of these modifications take place after conception and last until the end of the pregnancy. Increased cardiac output, increased blood volume, decreased blood pressure (BP), decreased systemic vascular resistance (SVR), and a slight increase in heart rate are among the hemodynamic changes associated with pregnancy [1]. Decrease in systemic vascular resistance in the first trimester triggers several compensatory mechanisms to maintain blood pressure, like an increase in cardiac output and plasma volume. In early normotensive pregnancy, both systolic and diastolic blood pressure decreased, reaching their maximum reduction in the second trimester. Then blood pressure gradually increased towards non-pregnant values [2]. Hormones have a major part within the preservation of physiological cardiovascular changes in pregnancy [3]. The cardiac output which is calculated as the (heart rate x the stroke volume) rises 30 to 50 percent (1.8 L/min) above baseline during normal pregnancy.
Increase in cardiac output results in part from changes in three important factors that determine it:
• Increase in the preload due to the increase in blood volume
• Decrease in afterload due to the decline in systemic vascular resistance
• Increase in heart rate.
In early pregnancy, increased cardiac output is primarily related to the rise in stroke volume. In late pregnancy, heart rate change is the major factor contributing to increased cardiac output [4]. SV started to grow during the first trimester and peaked between weeks 15 and 21 of pregnancy. Within the second half of the pregnancy, the increment in SV decrease and between 36 and 41 weeks of pregnancy SV did not contrast from that of non-pregnant ladies (2). Evidence has demonstrated that cardiovascular maladaptation happens in a large subset of women with preeclampsia (PE) or gestational hypertension (GH) [5]. Preeclampsia itself is defined as newly elevated blood pressure ≥ 140/90 after 20 weeks’ gestation in addition to proteinuria defined as 300 mg or more in a 24-h urine specimen, or a protein/creatinine ratio of 0.3 or more, or 2+ protein on urine dipstick (used if other quantitative methods are unavailable) [6,7]. The placenta releases too many anti-angiogenic factors into the mother's bloodstream during pre-eclampsia, which causes extensive endothelial damage and inflammation. There is evidence that this endothelial damage endures after the acute illness [8]. Women with a history of preeclampsia are at increased risk of cardiovascular morbidity and mortality.
Aim
Evaluation of some parameters of LV systolic and diastolic functions in preeclamic women and compare them with normotensive pregnancies.
Patient Selection and Methodology
This is case control study. Sixty women with single fetus- pregnancies ≥ 20 weeks’ gestation.
Patients referred and diagnosed by cooperation with obstetricians.
Exclusion criteria included: Smokers, women with history of chronic illness (as hypertension, diabetes mellitus, and heart failure), women with undetermined gestational age.
According to the diagnosis criteria of mild preeclampsia (which included elevated blood pressure ≥ 140/90 mmHg with 2 readings was at least 6hrs apart, proteinuria +2, with or without lower limb edema.
Patients were divided into 2 groups: Group 1: Preeclamptic group (n=30) and Group 2: Normotensive control group (n=30). Full history was obtained including age, menstrual and past history. Thorough clinical examination was performed recording height, weight, BMI, HR and ABP.
Maternal assessment was performed by a single examiner. The examination was done using echocardiography Device JE Vivid E9 through assessment of systolic function using Ejection fraction method and Simpson method with evaluation of diastolic function using transmitral Doppler flow method (the peak velocity of early (E), late (A) atrial filling and E/A ratio) and tissue Doppler method (To measure the early diastolic velocity (Em), and (E/Em) ratio ) for both preeclamptic and normotensive pregnant. The subjects were studied in left lateral decubitus position
Statistical analysis
Statistical Analysis: Data were analyzed using IBM SPSS Statistics, version 26. Independent t-tests were employed to compare the means of ejection fraction, E/A ratio, and E/Ee ratio between the study groups. A P-value of ≤ 0.05 was considered statistically significant.
Results
There was no statistically significant difference in Ejection Fraction (EF) between pre-eclamptic and normotensive pregnant women. The mean EF for pre-eclamptic women was 67.67%, compared to 65.37% in normotensive women (P=0.08), as shown in Fig. 1 and Tab. 1.
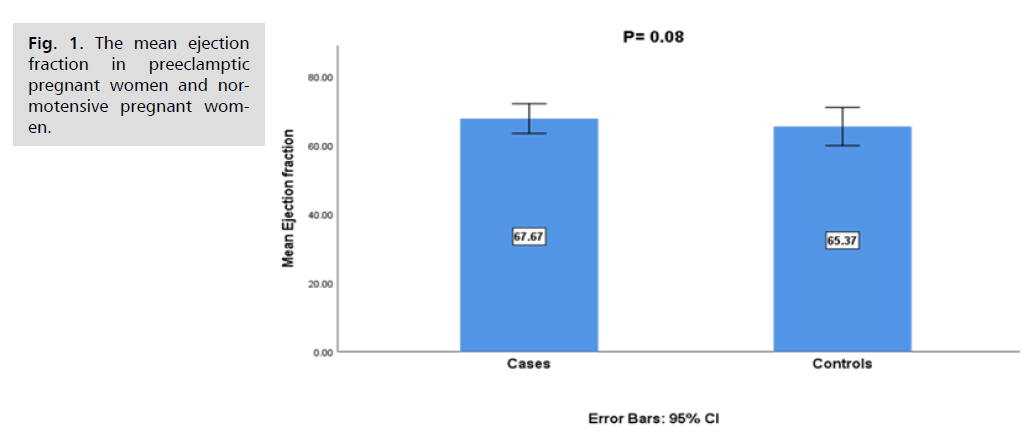
Fig. 1. The mean ejection fraction in preeclamptic pregnant women and normotensive pregnant women.
| Group Statistics | |||||
|---|---|---|---|---|---|
| Variables | Case or Control | N | Mean | Std. Deviation | Std. Error Mean |
| E/A ratio Diastolic Fuction of LV | case | 30 | 1.1200 | 0.20240 | 0.03695 |
| control | 30 | 1.1067 | 0.21324 | 0.03893 | |
| E prime lateral tissudoppllerof LV | case | 30 | 14.0000 | 2.72915 | 0.49827 |
| control | 30 | 15.6700 | 2.04048 | 0.37254 | |
| E/Ee ratio (E/Eprime ratio) diastolic function of LV by TDI | case | 30 | 5.01 | 1.942 | 0.355 |
| control | 30 | 4.00 | 1.247 | 0.228 | |
| Eprime septal | case | 26 | 10.8077 | 2.07883 | 0.40769 |
| control | 30 | 11.5667 | .85836 | 0.15671 | |
Tab. 1. The mean ejection fraction between pre-eclamptic and normotensive pregnant women.
The E/A ratio ranged from 0.80 to 1.60 with a mean of 1.113 ± 0.2062 across the entire sample of 60 participants. There was no significant difference in the mean E/A ratios between pre-eclamptic and normotensive women, with values of 1.11 and 1.12, respectively (P-value=0.8). As shown in Fig. 2., these findings indicate no significant difference in diastolic left ventricular function between the two groups.

Fig. 2. The mean of the E/A ratios of diastolic left ventricular function in preeclamptic pregnant women and normotensive pregnant women.
Fig. 3. shows that the E/Ee ratio was significantly higher in preeclamptic pregnancy [5] than in normotensive pregnancy [4], P=0.02. The minimum value of the E/Ee ratio across all participants was 1, the maximum value was 10, and the mean was 4.5 ± 1.70.

Fig. 3. The mean of the E/Ee ratios in preeclamptic pregnant women and normotensive pregnant women.
Discussion
We aimed to evaluate the effect of preeclampsia on some parameters of the systolic and diastolic function among pregnant women. We found that there were no significant differences between mild preeclamptic and normotensive women in systolic function as well as no statistically significant difference between them regarding E/A whereas there is statistically difference between two groups regarding E/Em ratio.
There was no significant statistically difference between both groups concerning the systolic function by trans-thoracic echocardiography as measured by ejection fraction likely due to the mild degree of preeclampsia among the study or small sample size.
Regarding diastolic functions, preeclamptic women had no a statistically significantly difference in E/A ratio from normotensive pregnant by conventional Doppler may be due to small sample size , there were significant difference between both groups as regarding E/Em ratio.
This study supports the hypothesis that changes in left ventricular diastolic functions may occur early in mild preeclampsia before hemodynamic disturbances (as changes in SV and SVR) which may occur late in severe preeclampsia. Echocardiographic screening for diastolic dysfunction may be helpful in predicting high-risk pregnancies [9]. Maternal echocardiography studies in preeclampsia have demonstrated significant cardiac dysfunction both before and at clinical onset of preeclampsia. Valensise, et al. first demonstrated that CO was significantly lower in early-onset (<34 weeks) preeclampsia compared with late-onset (≥ 34 weeks) preeclampsia [10]. Their findings were later confirmed and expanded on with the work of Melchiorre, et al [11]. Who showed that preeclampsia was also associated with abnormal cardiac geometry and diastolic dysfunction in the majority of women who developed preeclampsia. Differentiating features from normal pregnancy were left ve8ntricular wall thickness of ≥ 1.0 cm, exaggerated reduction in early diastole/atrial contraction, and lateral e′ of <14 cm/s which are the markers of diastolic dysfunction. Reduced stroke volume, diastolic dysfunction, and left ventricular remodeling are most marked in severe and early-onset preeclampsia and are associated with adverse maternal and fetal outcomes—irrespective of the conventional classification of preeclampsia based on clinical severity or gestation of onset [12-14].
Conclusion
This study revealed a significant impairment in the diastolic function of preeclamptic ≥20 weeks pregnant women compared to normotensive ones. However, it showed no significant difference as regards the systolic functions. This may suggest the significance of E/Em ratio to assess maternal cardiac functions and their prognosis in patients with mild preeclampsia.
Recommendations
We recommend large sample size for study diastolic dysfunction as a predictor of preeclampsia and follow patient in first 6 months after delivery.
References
- Nirupama R, Divyashree S, Janhavi P, et al. Preeclampsia: Pathophysiology and management. J Gynecol Obstet Hum Reprod. 2021 Feb 1;50(2):101975.
- de Haas S, Mulder E, Schartmann N, et al. Blood pressure adjustments throughout healthy and hypertensive pregnancy: A systematic review and meta-analysis. Pregnancy Hypertens. 2022;27:51-58.
- Kodogo V, Azibani F, Sliwa K. Role of pregnancy hormones and hormonal interaction on the maternal cardiovascular system: a literature review. Clin Res Cardiol. 2019;108:831-846.
- Spiegelman J, Meng ML, Haythe J, et al. Cardiovascular physiology of pregnancy and clinical implications. InCardio-Obstetrics 2020; CRC Press. 10-19.
- Gyselaers W. Hemodynamic pathways of gestational hypertension and preeclampsia. Am J Obstet Gynecol. 2022;226(2):S988-1005.
- Braunthal S, Brateanu A. Hypertension in pregnancy: Pathophysiology and treatment. SAGE Open Med. 2019;7:2050312119843700.
- Bisson C, Dautel S, Patel E, et al. Preeclampsia pathophysiology and adverse outcomes during pregnancy and postpartum. Front Med. 2023;10:1144170.
- Kirollos S, Skilton M, Patel S, et al. A systematic review of vascular structure and function in pre-eclampsia: non-invasive assessment and mechanistic links. Front Cardiovasc Med. 2019;6:166.
- Selim G, Sherief Mansour MD, Tamara M. Effect of Preeclampsia on Left Ventricular Diastolic Function. Med J Cairo Univ. 2022;90(9):1439-1443.
- Valensise H, Vasapollo B, Gagliardi G, et al. Early and late preeclampsia: two different maternal hemodynamic states in the latent phase of the disease. Hypertension. 2008;52(5):873-880.
- Melchiorre K, Sutherland G, Sharma R, et al. Mid-gestational maternal cardiovascular profile in preterm and term pre-eclampsia: a prospective study. BJOG. 2013;120(4):496-504.
- Vaught AJ, Kovell LC, Szymanski LM, et al. Acute cardiac effects of severe pre-eclampsia. J Am Coll Cardiol. 2018;72(1):1-1.
- Ferrazzi E, Stampalija T, Monasta L, et al. Maternal hemodynamics: a method to classify hypertensive disorders of pregnancy. Am J Obstet Gynecol. 2018;218(1):124-e1.
- Borges VT, Zanati SG, Peraçoli MT, et al. Maternal left ventricular hypertrophy and diastolic dysfunction and brain natriuretic peptide concentration in early-and late-onset pre-eclampsia. Ultrasound Obstet Gynecol. 2018;51(4):519-523.
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Author Info
Manal Yahya I. AL-Muhana1* and Amina A B AL Dujeli22Faculty of Medicine, University of Kufa, Kufa, Iraq
Copyright:This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.