Research - (2025) Volume 20, Issue 1
Hysteroscopy outcome evaluation in primary and secondary infertile women
Batool Abdulwahid Hashim Alkhalidi1*, Mays Sabah Al-saadi2, Shaymaa Raouf Tawfeeq1, Amal Muner Mubarak1, Fawz Alaa Alikhan1, Adnan A Al-Bdairi2 and Zainab Abdulkhadhim Fatnan1Received: 02-Jan-2025, Manuscript No. gpmp-25-158277; Editor assigned: 03-Jan-2025, Pre QC No. P-158277; Reviewed: 23-Jan-2025, QC No. Q-158277; Revised: 30-Jan-2025, Manuscript No. R-158277; Published: 31-Mar-2025
Abstract
Background: Uterine factor is a difficult contribution to female infertility that may seem like a hitch to gynecologists since it might compromise treatment outcomes by creating a hostile environment for embryo implantation, placentation, and fetal growth. When early tests show an abnormal uterine cavity, several institutions use hysteroscopy to diagnose and selectively treat diseases before giving IVF. Endometrial atrophy, synechiae, endometritis, polyps, FIGO 0-2 myomas, adenomyosis, septa, and other congenital anomalies are among the most common hysteroscopic findings, and this study was designed to map their distribution and disparity among patients.
Objectives: This study's objective is to is to survey and analyses types and frequencies of occurring of some hysteroscopy-detected uterine pathologies and the conception rate of primary and secondary infertile women who underwent hysteroscopic intervention to point the highest pregnancy rates of either infertile group.
Methodology: In the department of obstetrics and gynecology at the medical college of kufa university, this retrograde descriptive analysis was carried out for 100 infertile females’ cohort attended Al Zahra Teaching Hospital affiliated to Kufa university in Annajaf Al Ashraf province in Iraq over the period from Feb.2020 to June 2022, who underwent hysteroscopy intervention after written informed consent for assessment and or treatment of uterine factor for their primary or secondary infertility.
Results: Out of 100 patients included in the study, 66 (66%) presented with primary infertility and 34 (34%) presented with secondary infertility. Normal hysteroscopy were reported in 31 (31%) women, while intracavitory pathologies detected in the other 69 (or 69%) cases, these included endometrial polyp (48%) and uterine septum (26%), submucosal mayoma (14.5%), intrauterine synechiae (7%) and isthmocele (4%). In the patients with primary infertility, the abnormal hysteroscopic findings were reported in 41 (62%) women, in whom, the most common observed abnormality was endometrial polyp (51%), uterine septum (31%), and submucosal mayoma (14.5%). In patients with secondary infertility, the abnormal hysteroscopic findings were reported in 28 (82%) women and these were distributed as follow, endometrial polyp (43%) and uterine septum (18%), submucosal mayoma (14%), intrauterine synechiae (14%) and isthmocele (10%). The conception rate after treatment of abnormal uterine cavity pathology in primary and secondary infertile women were 29% and 39% respectively.
Conclusion: Given the results of the study, hysteroscopy should be strongly advised as a useful component in the management work up of infertile women particularly when intracavitery pathology is suspected by preliminary tests.
Keywords
Hysteroscopy; Primary infertility; Secondary infertility; Polyp; Uterine septum; Myoma; Isthmoceles; Synechae
Introduction
Infertility, it is the inability to achieve a clinical pregnancy after 12 months of regular, unprotected sexual activity as a result of a person's diminished ability to reproduce [1]. A clinical issue that affects 13% to 15% of couples globally [2]. There are two types of infertility: primary, in which there have been no prior pregnancies, and secondary, in which there has been a prior pregnancy but no live birth. 90% of couples should conceive after 12 months of unprotected intercourse in typical couples, and 50% of the population conceives after 3 to 4 months [3]. The frequency of infertility is on the rise today due to a number of factors, most important of which is both partners age. female factor constitutes 40–50% of infertility cases, such as ovulatory problems, tubal damage, however, uterine cavity pathologies are not infrequently encountered during evaluation of infertile women that it may be the sole problem or it is coexisted with other factors [4], thus, it is essential to evaluate and optimize the intrauterine environment in order to maximize the implantation rate of embryos. A variety of treatments have been suggested to treat infertility brought on by intrauterine diseases [5]. Compared to non-invasive methods like 2D, 3D Transvaginal Sonography (TVS), Hysterosalpingography (HSG), and Saline Infusion Sonography (SIS), hysteroscopy permits a more accurate detection of endometrial abnormalities; moreover, it permits the simultaneous treatment of an intrauterine pathology [6]. It has been stated that treating intrauterine pathologies with hysteroscopy improves reproductive outcomes. In numerous investigations, the advantages of employing interventional hysteroscopy to treat intrauterine diseases have been amply demonstrated [7,8]. Hysteroscopic and non-hysteroscopic interventions have been examined in several systematic and other designs studies [9-11], the probable difference in distribution of pathologies in patients with primary and secondary infertility, or whether hysteroscopy intervention is helpful in improving pregnancy rate in either type of infertility groups is currently studied.
Objective is to survey and analyze the conception rate of primary and secondary infertile women who underwent hysteroscopic intervention in addition to delineating the occurrence of normal and abnormal cavity by hysteroscopy and the difference in frequency of occurring of abnormal findings between two groups of patients.
Material and Method
Study design: This is a retrospective descriptive analysis. study population and setting; a 100 primary and secondary infertile women cohort, who underwent hysteroscopy in the Gynecology and obstetrics department in Al Zahra Teaching Hospital a teaching center affiliated to medical school of Kufa university at Annajaf Alashraf province in Iraq, over period from Feb. 2020 to June 2022, after obtaining ethical clearance from institutional ethical committee. Patients inclusion criteria are; all women with primary or secondary infertility with normal gonadotropin hormone values having their husbands with normal semen analyses, patients 18- 40 years of age with suitable AMH level in whom (patient exclusion criteria) no contraindication for hysteroscopy, no abnormal vaginal bleeding or possibility of pregnancy, sever cardio-pulmonary compromise or active and overt pelvic infection, other excluded patients are those patients, who refused surgery, couples with moderate to severe male factor infertility, couples who had not been together for 12 months, patients not achieving criteria of definition either primary and secondary infertility, Patients with high basal serum Follicle Stimulating Hormone (FSH) level, women using an intrauterine device, incomplete or failed hysteroscopic entry or deficient patients’ data. All patients were followed for variable period ranging from 3-16 months for clinical pregnancy if occurred either spontaneous, ovulation induction with timed intercourse or with (OI/TI) or intrauterine insemination IUI/ICSI.
Technique: In our center, all patients were interviewed one day before surgery during the proliferative phase of menstrual cycle (as possible), their records were reviewed regarding their history, examination, investigation like hormonal assay and TSH function. pre-anesthetic examination was performed, preoperative vaginal synthetic prostaglandin 400 mcg 2-4 hours before procedure. Diagnostic and therapeutic hysteroscopy conducted under light general or spinal anesthesia, bimanual pelvic examination was carried out with the patient in the high lithotomy position, upper cervical lip was grasped using Vulsellum forceps once the cervix visualized using two vaginal Sim's speculae, hysteroscopy was introduced into the uterine cavity the endocervical canal inspected, cavity, both ostia, the right and left cornua, fundus, anterior, posterior, and lateral walls, were inspected systematically for particular lesions. {Complete (complete examination of the entire uterine cavity, including both ostia), incomplete (examination of the entire uterine cavity not possible, for example, lesions), and unsuccessful (the surgery was not successfully completed) (examination of the uterine cavity not possible}). Detected lesions all were treated with either scissors or to resectoscope whenever needed
Device criteria: A 2.9 mm and 30˚ diagnostic single-flow hysteroscopy were used for all surgeries. a 5 mm single flow sheath with an integrated irrigation channel and an II rod lens telescope from Karl Stores. A high-intensity cold light source was used to illuminate the workspace via a fiberoptic link, and a video camera and monitor were used to keep an eye on all operations. As a medium, normal saline was selected. The pressure was pre-settled to 80–100 mmHg. Hysteroscopy was performed using a continuous flow 30o rigid operating hysteroscopy with a diameter of 5 mm. therapeutic hysteroscopy (21 French) resectoscopy loop bipolar diathermy (Karl Stores), information was gathered from the patient files, tabulated, and analyzed, patients were contacted for any missed information, all hysteroscopic procedures were done by a single gyn. Ob. Surgeon (Batool A. Hashim) who has more than 5 years’ experience of gyn. endoscopic surgery.
Statistical analysis: Statistical Package for Social Sciences and Microsoft Excel were used to enter the data. SPSS version 10.0 is used to statistically to analyze and code the data. Continuous variables were summarized in the form of mean and standard deviation. Categorical variables were summarized as percentage. Frequency distribution tables, p value of <0.05 was considered statistically significant.
Results
Of 100 infertile patients included in this study, 66 (66%) women with primary infertility and 34 (34%) with secondary infertility, as illustrated in Fig. 1. The figure describes our patient’s algorithm uterine pathologies were diagnosed in 69 of 100 infertile women, the frequency of their occurrence in our population study; endometrial polyp33(48%), septa 18(26%), FIGO 0&1 myoma10 (14.5%), Intrauterine synechia 5(7%), and isthmoceles in 3 cases (4%) (Fig. 2.).
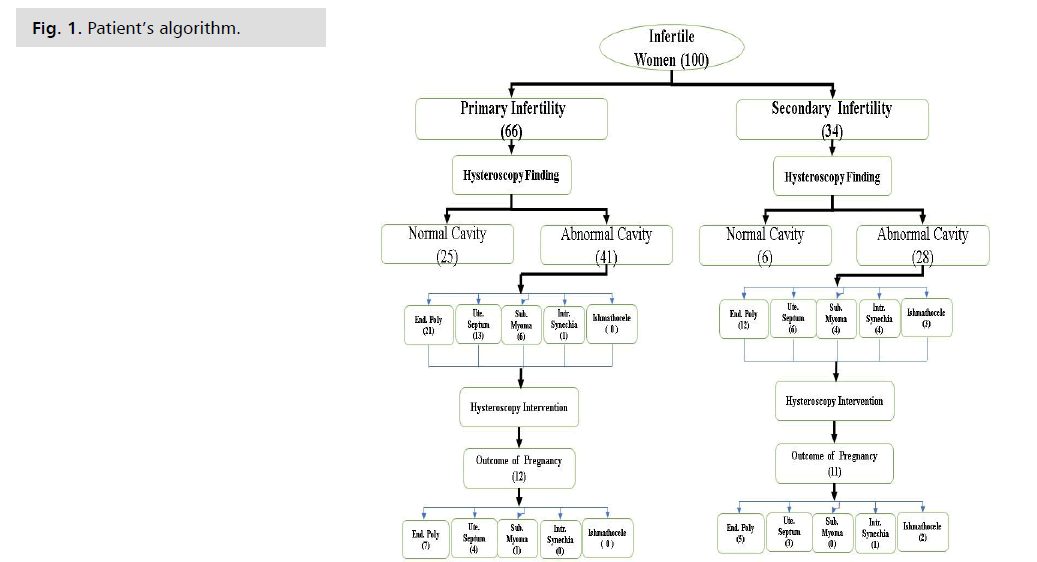
Fig. 1. Patient’s algorithm.
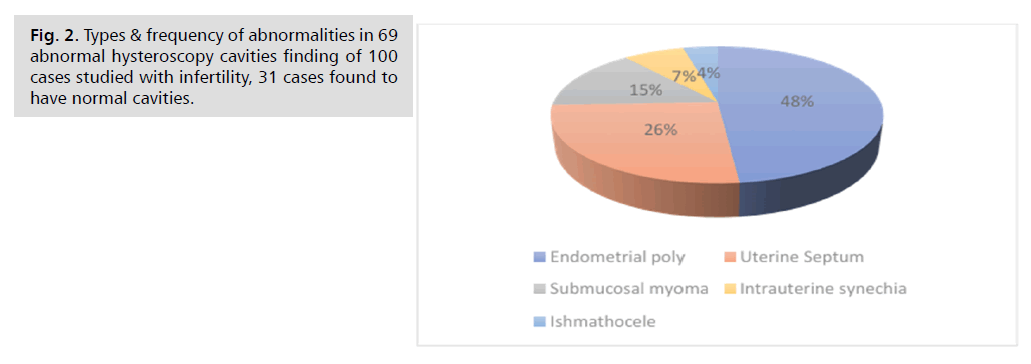
Fig. 2. Types & frequency of abnormalities in 69 abnormal hysteroscopy cavities finding of 100 cases studied with infertility, 31 cases found to have normal cavities.
Although there was statistical significance in mean age of patients with primary and secondary infertility, (31.44 ± 6.7 vs. 34.3 ± 7.3) in our population sample, however; duration of infertility was not significantly different between neither of them (Tab. 1.).
| Patients | Primary Infertility (years) | Secondary Infertility (years) | P Value |
|---|---|---|---|
| Mean age ± SD | 31.44 ± 6.7 | 34.3 ± 7.3 | 0.05# |
| Mean of inf. duration ± SD | 9.3 ± 5 | 7.8 ± 4.4 | 0.14 |
| #Statistically Non-significant (P-value <0.05) | |||
Tab. 1. Mean ± standard deviation of age and infertility duration for primary and secondary infertile women.
In our population studied, of 66 primary infertility sufferers 41(62%) were found to have pathologies diagnosed by hysteroscopy these were according to their frequency of occurring, endometrial polyps 21(51%), uterine septum 13(31%), submucosal myoma 6(14.5%), and one case of intrauterine adhesions (0.02%) (Tab. 2.).
| Hysteroscopy Findings | Total | Primary Infertility | Secondary Infertility | P- value | |||
|---|---|---|---|---|---|---|---|
| No. | % | No. | % | No. | % | ||
| Total | 100 | 100% | 66 | 66% | 34 | 34% | 0.03 |
| Normal Cavity | 31 | 31% | 25 | 37% | 6 | 18% | |
| Abnormal Cavity | 69 | 69% | 41 | 62% | 28 | 82% | |
| Endometrial polyp | 33 | 48% | 21 | 51% | 12 | 43% | 0.1 |
| Uterine Septum | 18 | 26% | 13 | 31% | 5 | 18% | |
| Submucosal myoma | 10 | 14.50% | 6 | 14.50% | 4 | 14% | |
| Intrauterine synechia | 5 | 7% | 1 | 0.02% | 4 | 14% | |
| Ishmothocele | 3 | 4% | 0 | 0% | 3 | 10% | |
Tab. 2. Hysteroscopic intraoperative findings.
The figures for patients with secondary infertility; of total 34 women, 28(82%) were diagnosed with uterine pathologies and these were according to their frequency 12 (43%) polyps, 5(18%) cases with uterine septa, 4(14%) for myoma and intrauterine synechae, and 3(10%) cases with CS scar defects (isthmoceles), abnormal cavity finding in both primary and secondary infertile women was statistically significant (P- value=0.03).
After hysteroscopic treatment of uterine pathologies, for women with primary infertility 12 of 41 (29%) achieved clinical pregnancy after 3-18 months of patients follow up, and 11 of 28 (39%) of those with secondary infertility had achieved clinical pregnancy within same period of follow up (Tab. 3.)
| Cavity Abnormal Finding | Primary pregnancy Outcome (12) | Primary conception rate 100% | Secondary Pregnancy Outcome (11) | Secondary Conception rate 100% | Total pregnancy Outcome (23) | Total Conception rate 100% | P-value |
|---|---|---|---|---|---|---|---|
| Endometrial poly | 7 | 58% | 5 | 45.50% | 12 | 52% | 0.8 |
| Uterine Septum | 4 | 33.50% | 3 | 27.50% | 7 | 30.50% | |
| Submucosal myoma | 1 | 8.50% | 0 | 0% | 1 | 4.50% | |
| Intrauterine synechia | 0 | 0% | 1 | 9% | 1 | 4.50% | |
| Ishmothocele | 0 | 0% | 2 | 18% | 2 | 8.50% | |
| Total | 12 | 100% | 11 | 100% | 23 | 100% |
Tab. 3. Clinical pregnancy rate for those.
Most of those who conceived in both groups of primary and secondary infertility were following hysteroscopic polypectomy (58% vs. 45.5%), and septolysis (33.5% vs. 27.5%)consequently, with no statistical significance between two groups, worth mentioning that 27% of patient with secondary infertility conceived after treatment of (CS scar defect 2 cases and one case of peripheral cavity adhesiolysis of endometrial synechae) previous childbirth complications (Tab. 4.).
| Cavity Abnormal Finding | Primary pregnancy Outcome (12) | Primary conception rate 100% | Secondary Pregnancy Outcome (11) | Secondary Conception rate 100% | Total pregnancy Outcome (23) | Total Conception rate 100% | P-value |
|---|---|---|---|---|---|---|---|
| Endometrial poly | 7 | 58% | 5 | 45.50% | 12 | 52% | 0.8 |
| Uterine Septum | 4 | 33.50% | 3 | 27.50% | 7 | 30.50% | |
| Submucosal myoma | 1 | 8.50% | 0 | 0% | 1 | 4.50% | |
| Intrauterine synechia | 0 | 0% | 1 | 9% | 1 | 4.50% | |
| Ishmothocele | 0 | 0% | 2 | 18% | 2 | 8.50% | |
| Total | 12 | 100% | 11 | 100% | 23 | 100% |
Tab. 4. Pregnancy rate of abnormal cavity finding after treated by hysteroscopy.
Discussion
Evaluation of endometrium and uterine cavity has long been regarded as an essential step of management of female infertility as they largely affect receptivity and subsequent embryo implantation and development [12]. In spite of normal initial imaging modalities (hysterosalpingography and 2-D sonography) that are used in initial infertility patients -workup, hysteroscopy still can disclose uterine abnormalities in considerable proportion of them approaching 38.8% in some studies [12,13]. Uterine pathologies like endometrial polyps, submucus myomas, uterine septa, Caesarean scar defects and intrauterine adhesions are among the commonest hysteroscopic disclosures that made some authors recommend the latter as a routine investigative tool for women with primary and secondary infertility [14,15]. In the current study, of 100 women, 66 (66%) have primary infertility and 34 (34%) have secondary infertility a figure which was so close to that of Sharma P, et al. [16], who’s population study sample that they evaluated by hysterolaparoscopy was 76 cases of them 64% were with PI and 36% were with SI. Our mean patient age and duration of infertility was (31.44 ± 6.7, 34.3 ± 7.3) and (9.3 ± 5, 7.8 ± 4.4) years for patient with primary and secondary infertility consequently, abnormal intrauterine findings were seen in 41/66(62.1%) and 28/34 (82%) i. e. in our study it was more likely to have abnormal pathology in patient with secondary than primary infertility a finding that was inconsistent with that of Rakholia R, et al. [17], who encountered no statistical significant difference in finding abnormal pathology in patients with PI and SI (51.9% and 46.3%), this may be explained by relatively elder mean patients age in our study compared to their study, as majority of patients with PI (41% ) were 20-25 years, and for SI most patients(53.7%) were 26-30 years old in his study [17], while our mean age were 31.44 ± 6.7 and 34.73 ± 7.3 for PI and SI respectively. In our study, 33/69 (48%) of pathologies were endometrial polyps, however; this percentage varies widely among different studies, lowest seen in 0.05% by Nayak PK, et al. [18] to 20% by Venus BDS, et al. [19], reaching up to 36.66% by Jain T, et al. [14] and that it was worth noticing that studies combined hysterolaparoscopy may were under-reporting polyps, focusing on frequently coexisted gross pelvic pathologies, like endometriosis, pelvic/ tubal, cervical infective diseases [20]. Infertility and endometrial polyp association has been extensively explained by being both mechanical and molecular effects, this are by interfering with sperm ascent, covering progesterone –responsive implantation site, inducing local inflammation and chronic inflammatory cells infiltration and release of matrix metalloproteinase 2&9, endometrial polyp also reduces mRNA level of HOXA10and HOXA11, two famous markers of receptive endometrium [21].
Submucosal myoma is reported in equal frequencies for both PI&SI, (14.5%) in this study, and literatures review concluded that hysteroscopic resection of FIGO 0-1 myoma would benefit women with unexplained infertility [22,23].
18/69 (26%) of intracavitary lesions were uterine septa (31% vs. 18%) with prevalence higher in primary than secondary infertility, a finding that agrees with most other studies [14,16-19], while Gandotra N [24], reported septum in 6.1% vs. 3% in SI &PI respectively. The way that uterine septa influence individual woman fertility, and outcomes of their hysteroscopic management had been discussed in details in our case series of (outcomes of hysteroscopic septolysis).
Unsurprisingly, there were also higher incidence of Intrauterine Synechae (IUS) in patients with SI (14%) vs. (0.02%) in patients with PI, as they are caused by irreversible damage to basal layer of endometrium usually following peripartum/ abortion intrauterine procedures. IUS leads to partial or complete adhesion inside the uterine cavity that can present with hypo/amenorrhoea, pelvic pain, abortion, and infertility. Hysteroscopic adhesiolysis has revolutionized both its diagnosis and treatment, European Society of Gynecological Endoscopy (ESGE) guidelines recommend using cyclic estrogen-progestin therapy after TCRA to promote endometrial growth and repair after hysteroscopic Transcervical Resection of Adhesions (TCRA) [25] a policy that is also followed by the author. Isthmoceles 3/69(4%) (0% vs. 10%) for PI&SI consequently. Theoretically, the lower uterine segment is having a poor vascularity a fact that may retard caesarean scar healing thus scar area may get partial dehiscence creating a defect that is known as isthmocele [26]. The association between isthmoceles and difficulty in conception is now documented [27], however; the exact mechanism is yet to be fully understood. The most proposed mechanism is presence of embryotoxic effect of accumulated blood and hemoglobin iron inside the defect [28], impaired endometrial receptivity by chronic microbial infection [29], surgical correction of CS scar defects will restore normal anatomy and reverse hydrometra [30]. Isthmocele can entrap sperms and interfere with their ascent mechanically, and provide gametotoxic environment to their survival and functions [31].
In our study, total cases of clinical pregnancy were 23(33.3%) and was higher for patients with SI compared to PI patients 39% s29% respectively, that was close to figure of 31.18% given by Rakholia R, et al. [17]12cases after polypectomy, 7concieved after septolysis, 2 after CS scar defect hysteroscopic repair, 1 after adhesiolysis and 1 after hysteroscopic myomectomy, 18 of 23 were conceived by ICSI, 2 after ovulation induction / timed intercourse (OI/TI), and 3 patients conceived spontaneously after septolysis in period ranging from 3-9 months.
Conclusion
Hysteroscopy seems to be safe and effective diagnostic and therapeutic option in management of women with infertility, it can enhance their clinical pregnancy treatment outcomes by addressing subtle and gross acquired and congenital lesions, thus it needs to be involved in female infertility assessment and workup earlier, and to lower the threshold of recourse to hysteroscopy in subfertile women to prevent the unnecessary wastage of the limited fertile women age.
Future Study
• Estimate these enzymes for infertility patients after the seminal fluid analysis.
• 2-Study the effects of seminal plasma enzymes in the female reproductive system on the capacitation, hyper activation and acrosome reaction.
References
- Zegers-Hochschild F, Adamson GD, Dyer S, et al. The international glossary on infertility and fertility care, 2017. Hum Reprod. 2017;32(9):1786-1801.
- Kamel RM. Management of the infertile couple: An evidence-based protocol. Reprod Biol Endocrinol. 2010; 8:21.
- Gnoth C, Godehardt E, Frank-Herrmann P, et al. Definition and prevalence of subfertility and infertility. Hum Reprod. 2005;20(5):1144-1147.
- Monga A, Dobbs SP. Gynaecology by ten teachers. CRC Press. 2011.
- Iris A, Aydogan Kirmizi D, Taner CE. Effects of infertility and infertility duration on female sexual functions. Arch Gynecol Obstet. 2013;287:809-812.
- Bajaj M, Roy R, Rahman M, et al. Hysteroscopy is Gold standard in Uterine evaluation for Infertility, but HSG still has a place. Asian J Med Sci. 2021;12(4):98-104.
- Di Spiezio Sardo A, Di Carlo C, Minozzi S, et al. Efficacy of hysteroscopy in improving reproductive outcomes of infertile couples: A systematic review and meta-analysis. Hum Reprod. 2016;22(4):479-496.
- Chiofalo B, Palmara V, Vilos GA, et al. Reproductive outcomes of infertile women undergoing “see and treat” office hysteroscopy: A retrospective observational study. Minim Invasive Ther Allied Technol. 2021;30(3):147-153.
- Pundir J, Pundir V, Omanwa K, et al. Hysteroscopy prior to the first IVF cycle: A systematic review and meta-analysis. Reprod BioMed. 2014;28(2):151-161.
- Mao X, Wu L, Chen Q, et al. Effect of hysteroscopy before starting in-vitro fertilization for women with recurrent implantation failure: A meta-analysis and systematic review. Medicine. 2019;98(7):e14075.
- Dur R, Ahat B, Yılmaz AY, et al. The effect of hysteroscopy on fertility in women with unexplained infertility. Galen Med J. 2024;35:387-392.
- Elbareg AM, Essadi FM, Anwar KI, et al. Value of hysteroscopy in management of unexplained infertility. Asian Pac J Reprod. 2014;3(4):295-298.
- Barati M, Zargar M, Masihi S, et al. Hysteroscopy in Infertility. Int J Fertil Steril. 2009;3:17-20.
- Jain T, Dutta S, Gupta M, et al. Hysteroscopy: An Essential Tool in the Workup of Infertility. Int J Infertil Fetal Med. 2023;14(2):100-104.
- Mitwally AB, Badran EY, Arby T, et al. Evaluation of the uterine cavity by office hysteroscopy in patients with infertility and recurrent pregnancy loss: A cross sectional study. Int J Reprod Contracept Obstet Gynecol. 2019;8(1):201.
- Sharma P, Jhanwar A, Kumari K, et al. A Prospective Study to Evaluate the Role of Combined Diagnostic Laparoscopy and Hysteroscopy in the Management of Female Infertility. Cureus. 2024;16(1).
- Rakholia R, Donthu K, Sinha S, et al. Efficacy of combined hysteroscopy and laparoscopy in the evaluation and management of female infertility at a tertiary care center. Int J Reprod Contracept Obstet Gynecol. 2024;13(10).
- Nayak PK, Mahapatra PC, Mallick JJ, et al. Role of diagnostic hystero-laparoscopy in the evaluation of infertility: A retrospective study of 300 patients. J Hum Reprod Sci. 2013;6(1):32-34.
- Venus Bansal DS, Bhavani BH, Avasthi K, et al. To study the role of diagnostic hysterolaparoscopy in the evaluation of infertility. Int J Clin Obstet Gynaecol. 2023;7(6):27-34
- Shah SJ, Murrium SK, Naveed F, et al. Gynaecological Polyps Causing Infertility-A systemic review. Pak J Med Health Sci. 2022;16(01).
- Terzic M, Dotlic J, Vasiljevic M, et al. Endometrial polyps in infertility patients: The first study of their clinical characteristics. Clin Exp Obstet Gynecol. 2018;45(5):2018.
- Bosteels J, Kasius J, Weyers S, et al. Hysteroscopy for treating subfertility associated with suspected major uterine cavity abnormalities. Cochrane Database Syst Rev. 2015;2:CD009461.
- Izhar R, Husain S, Tahir S, et al. Fertility outcome after saline sonography guided removal of intrauterine polyps in women with unexplained infertility. J Ultrasonography. 2019;19(77):113-119.
- Gandotra N. Role of diagnostic hysteroscopy in establishing the diagnosis of female infertility. Int J Clin Obstetr Gynaecol. 2018;2(6):27-30.
- Feng L, Sun Y, Zhang S, et al. A novel intrauterine estrogen-releasing system for preventing the postoperative recurrence of intrauterine adhesion: A multicenter randomized controlled study. BMC Med. 2024;22(1):395.
- Joshi JS, Potdar J, Shanoo A, et al. Cesarean Scar Ectopic Pregnancy: A Rare Case. Cureus. 2024;16(2).
- McGowan S, Goumalatsou C, Kent A. Fantastic niches and where to find them: The current diagnosis and management of uterine niche. Facts Views Vis Obgy. 2022;14(1):37.
- Bij de Vaate AJ, Van der Voet LF, Naji O, et al. Prevalence, potential risk factors for development and symptoms related to the presence of uterine niches following Cesarean section: Systematic review. Ultrasound Obstet Gynecol. 2014;43(4):372-382.
- Moreno I, Simon C. Relevance of assessing the uterine microbiota in infertility. Fertil Steril. 2018;110(3):337-343.
- Ahamed FM, Solkar S, Stevikova M, et al. Link between cesarean section scar defect and secondary infertility: Case reports and review. JBRA Assist Reprod. 2023;27(1):134.
- Baldini GM, Lot D, Malvasi A, et al. Isthmocele and Infertility. J Clin Medicine. 2024 Apr 10;13(8):2192.
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Google Scholar, Cross Ref, Indexed at
Author Info
Batool Abdulwahid Hashim Alkhalidi1*, Mays Sabah Al-saadi2, Shaymaa Raouf Tawfeeq1, Amal Muner Mubarak1, Fawz Alaa Alikhan1, Adnan A Al-Bdairi2 and Zainab Abdulkhadhim Fatnan12Teba Medical Center, Babylon, Iraq
Copyright:This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.