Research - (2023) Volume 18, Issue 2
Criteria of women with best outcome after using vaginal misoprostol for termination of 1st trimester missed abortion
Hameed Jameel Hamzah1, Russul Daad Abd Oun1, Tahsin Hadi Husain1, Akhlas Hashem Salman1* and Al-Sharifi AZ2Received: 25-Apr-2023, Manuscript No. gpmp-23-96957; Editor assigned: 26-Apr-2023, Pre QC No. P-96957; Reviewed: 10-May-2023, QC No. Q-96957; Revised: 17-May-2023, Manuscript No. R-96957; Published: 30-Jun-2023
Abstract
Background: Missed abortion is a gestational sac containing a dead embryo without clinical symptoms of expulsion (death and retention). Misoprostol is a synthetic prostaglandin analog that has been shown to stimulate uterine contractility in early pregnancy.
Objective: This study aims to decide the characteristics of the patient that got greater benefit from using misoprostol in termination of 1st-trimester missed abortion, taking into consideration the limitations of using misoprostol and the possible adverse reactions.
Methods: A single-blind clinical trial was performed in the Obstetrics and Gynecology Department of Al-Yarmouk Teaching Hospital. Totally, 133 patients with 1st trimester missed abortions were referred from our consultant clinic. Were detailed history and full medical and obstetric examinations were carried out. The demographic characteristic of each patient was assessed including Age (years), body weight, gravidity, parity, history of previous abortion, previous uterine scar, previous medical disorders, any vaginal bleeding, and gestational age that was determined by LMP and U/S. Our study regimen by using misoprostol as a monotherapy to ripen and dilate the cervix before surgical evacuation, or achieve complete medical abortion. Following a digital vaginal examination, a (400 µg) Misoprostol tablet was inserted.
Results: The mean age of patients was (25.99) years and the mean body mass index was within the normal range. Twenty-eight out of ninety-five (29.4%) were primigravida and 71.6% (67 out of 95 patients) were multigravida; eight of them had a history of previous uterine scar and 17 of the multigravida women had a history of surgical abortion. The obstetrics history and examination revealed that the median gestation age was 10 weeks (assessed by the last menstrual period) or 8 weeks (assessed by ultrasonography). Closed cervical oss was observed in 47 out of 95 cases (49.5%) and the minority presented with vaginal bleeding (9.5%). The majority of patients received either one dose (400 µg), two doses (800 µg), or three doses (1200 µg). The endpoint effects of misoprostol were observed in terms of cervical dilatation, vaginal bleeding, and the expulsion of gestation products. Complete expulsion of gestation product was observed in 38 out of 95 cases (40%) with different doses and times.
Conclusion: Younger age, low BMI, multi parity, initial cervical dilatation, short time fetal death as well as absent previous history of uterine scar, all are the criteria of the patient with the best outcome when using misoprostol vaginally for 1st trimester missed abortion and can be a reliable predictor to uterine response for vaginal misoprostol when used for 1st trimester missed abortion. Intra-vaginal misoprostol alone as monotherapy at a dose of 400 µg every 6 hours is an effective regimen to achieve successful termination of 1st trimester missed abortion. Moistening of misoprostol by normal saline is more effective than dry misoprostol. 2nd and 3rd dose effectiveness of misoprostol was observed. The adverse effects of misoprostol are minimal and dose-related and self-limiting.
Keywords
Miscarriage; Misoprostol; 1st Trimester missed abortion; Pregnancy termination
Introduction
Miscarriage is the most common complication of pregnancy. A proximately 50% of all conceptions and 5% of all recognized pregnancy result in miscarriage. The world health organization defined miscarriage as "expulsion or extraction from its mother of an embryo or fetus weighing 500 gm or less [1,2]. Early pregnancy loss, is defined as a loss within 12 completed weeks of pregnancy that occurs in 10 – 20% of clinical pregnancies and is responsible for about 50000 patient admission in the UK annually [3]. The most common types of early pregnancy failure include spontaneous miscarriage (complete and incomplete), embryonic gestation, and embryonic or fetal death [4].
Misoprostol is a synthetic prostaglandin E1 analog marketed as an oral preparation used to prevent and treat gastro-duodenal damage induced by non-steroidal anti-inflammatory drugs (NSAIDs). Misoprostol has been shown to stimulate uterine contractility in early pregnancy [5] and at term [6]. Administered orally or vaginally, it is effective for inducing abortion [7,8] and labor [9], though it poses certain risks [10]. Apart from its uterotonic effects, misoprostol has known pharmacologic effects on several organ systems. It inhibits platelet-activating factors and affects metabolic and physiological processes, including thermoregulation [11]. Life-threatening hyperpyrexia has been reported following the use of misoprostol, 800 µg orally, after childbirth [12].
Misoprostol's effects are dose-dependent and include cervical softening and dilation, uterine contractions, nausea, vomiting, diarrhea, fever, and chills [13].
There is no doubt that misoprostol had been used under the heading of medical abortion in many centers and hospitals? Its efficacy was assessed as a useful remedy on this occasion whether as mono-therapy or add-on therapy. This study aims to decide the characteristics of the patient that got greater benefit from using misoprostol in termination of 1st-trimester missed abortion, taking into consideration the limitations of using misoprostol and the possible adverse reactions.
Methods
Study design and settings
A single-blind clinical trial was performed in the Obstetrics and Gynecology Department of Al-Yarmouk Teaching Hospital in Baghdad Iraq between the 1st of June 2018 and to end of May 2020. This study is approved by The Scientific Council of Obstetrics and Gynecology as a requirement for Fellowship of The Iraqi Board of Obstetrics and Gynecology.
Inclusion criteria
• Reproductive age gropes.
• Gestation age 12 weeks.
• Ultrasound confirmed the diagnosis of missed miscarriage.
• Good past health.
• No contraindications for using misoprostol.
Exclusion criteria
• Severe blood loss.
• Sepsis.
• Allergy to prostaglandins.
• Ultrasound findings of extrauterine pregnancy.
• Severe liver and renal impairment.
• History of severe asthma.
Study groups
Totally, 133 patients with 1st trimester missed abortion were referred from our consultant clinic in Al-Yarmouk Teaching Hospital or a private clinic, and admitted to the obstetric and gynecologic department, unfortunately (38) of them were excluded from our analysis (for different causes) as much as (95) patient who met the criteria of inclusion were collect into this study.
All the patients agreed to participate in this study and verbal consent was obtained from every patient included in the study.
Were detailed history and full medical and obstetric examinations were carried out.
The demographic characteristic of each patient was assessed including Age (years), body weight, gravidity, parity, history of previous abortion, previous uterine scar, previous medical disorders, any vaginal bleeding, and gestational age that was determined by LMP and U/S.
Each patient was assessed clinically before and after misoprostol therapy from the following points of view:
1. Previous uterine incision.
2. Trans abdominal ultrasonography on admission (looking for a missed carriage, incomplete miscarriage, cervical dilatation, gestation age).
3. Primary response (cervical state), and the time of response.
4. Time of expelled gestation.
5. Total number of doses.
6. Add on surgical abortion.
7. Hematocrit.
8. Post-medical abortion ultrasonography.
9. Tolerance.
Routine investigations were conducted for each patient including:
(Complete blood picture, blood group, and RH, serum fibrinogen level, platelets count by our hospital lab facility). Patients with U/S outside the hospital rescan in our hospital to confirm the diagnosis. For many patients, a double ultrasound scan was taken one week apart to confirm fetal death. As I mentioned in chapter one, there are three regimens for medical abortion (mifepristone & misoprostol, methotrexate & misoprostol, or misoprostol only).
Our study regimen by using misoprostol as a monotherapy to ripen and dilate the cervix prior to surgical evacuation, or achieve complete medical abortion.
Following digital vaginal examination (for assessment of cervical state﴿ a (400 µg) Misoprostol tablet was inserted (in one of two ways either moistened in normal saline 80 pt or not moistened 15 pt) in the posterior vaginal fornix at 6 h intervals for a maximum of 4 doses within 24 h. which was supervised by registrar doctor, follow up the case and is further managed by the resident doctor on call.
During this period of observation, no additional drugs were given, unless indicated (as analgesia for pain).
The patient was clinically assessed at the following points:
a) Clinical observation (every four hours) includes the record of blood pressure, pulse rate, temperature, and the dose of analgesia given.
b) Early response (cervical state).
c) Expulsion of gestational products.
d) Side-effects: nausea, vomiting, abdominal pain, diarrhea, dizziness, fatigue, pain, headache, breast tenderness, chills or hot flushes, excessive bleeding.
e) The time of the expulsion of the conceptus (induction expulsion period).
f) Post-treatment vaginal bleeding.
A pint of crossed-matched blood was prepared for all the patients and given if necessary.
When abortion started and the expulsion of the fetus occurred, we see whether the abortion was complete or not by PV examination and the US.
Pethidine hydrochloride 1 mg/kg (up to 100 mg) by intramuscular injection, tramadol, and Diclofenac sodium was given for pain relief if requested by the patient.
If the patient does not respond after (24) hrs of treatment further course of misoprostol was given in 2nd (24) hrs unless the patient required surgical evacuation (if heavy bleeding).
Before the next dose is given cervical status were assessed by vaginal examination, when abortion is imminent there is no need for further doses, & patients are referred from word to the labor room and prepared for surgical evacuation under general anesthesia (if abortion is not completed), some of them get complete expulsion during waiting the operation time, others need surgical evacuation by curettage, the process of evacuation was performed easily with no much harm to the cervix because it was already ripe due to effects of misoprostol, no perforation, no bleeding due to uterotonic effects of misoprostol.
All patients then followed up for 24 h post-abortion to monitor immediate post-abortion complications with monitoring of vital signs, any systemic symptoms and vaginal bleeding, or any passage of product of conceptus per vagina.
Ultrasound examination was performed to detect any retained product of conception for those patients who had no complete abortion, those women with an empty uterus after misoprostol treatment were discharged, those who still had a significant part of a product of conception (> 2.5 cm) with vaginal bleeding had an evacuation of a retained product under general anesthesia and then discharged.
Those who still had a product of conception (˂ 2.5 cm) with no, or slight vaginal bleeding were discharged and continued on the same dose at home.
Before discharge each patient was instructed to report any abdominal pain or discomfort, vaginal bleeding, fever, general malaise, and passage of any tissue mass vaginally, if any of these symptoms occurred, they asked to return to the hospital.
Some of them get completely expulsion at home and returned to the hospital, U/S was done to confirm complete expulsion. If the patient's blood type was Rh negative, she received anti-D.
The primary outcome measurements are:
1. Cervical dilatation & vaginal bleeding.
2. A total dose of misoprostol.
The drug was stopped under one of the following conditions:
1. Severe vaginal bleeding.
2. Cervical dilatation.
3. Complete expulsion of the conceptus.
The endpoint of the assessment is to look for:
a. Duration of vaginal bleeding.
b. Dosage of analgesics requirement.
c. Occurrence of infection.
d. Patients' acceptability.
e. The need for surgical curettage.
Statistical analysis
The results are presented as number, percent, and whenever possible as mean ± SD. The data were analyzed using Student's "t" test (unpaired, two-tailed) and Chi-squared test taking the p≤ 0.05 as the lowest limit of significance.
Results
Tab. 1. shows the characteristics of patients enrolled in the study. The mean age of patients was (25.99) years and the mean body mass index were within the normal range. Twenty-eight out of ninety-five (29.4%) were primigravida and 71.6% (67 out of 95 patients) were multigravida; eight of them had a history of previous uterine scar and 17 of the multigravida women had a history of surgical abortion. Chronic medical illnesses were diabetes mellitus (3 cases) and hypertension (2 cases).
| Variables | No. (%)/mean ± SD |
|---|---|
| Age | 25.99 ± 4.36 |
| BMI (kg/m2) | 26.70 ± 1.260 |
| Parity | |
| Null | 28 (29.47) |
| Para 1 | 25 (26.31) |
| Para 2 | 17 (17.89) |
| Para 3 | 17 (17.89) |
| Para 4 | 05 (5.26) |
| Para 5 | 03 (3.15) |
| History of previous pelvic scar | 08 (8.42) |
| Previous history of abortion | 28 (29.47) |
| Previous history of surgical abortion | 17 (17.89) |
| History of Diabetes Mellitus | 03 (3.15) |
| History of hypertension | 02 (2.10) |
Tab. 1. The characteristics of pregnant women.
On admission, the vital signs other than the packed cell volume were within acceptable normal ranges (Tab. 2.). The mean respiratory rate was 16.4 breaths per min, the mean body temperature was 37.05°C, and the mean systolic and diastolic blood pressures were 117.47 and 66.63 mmHg respectively.
| Variables | Before treatment | After treatment |
|---|---|---|
| Packed cell volume | 0.350 ± 0.017 | 0.320 ± 0.023 |
| Respiratory rate (cycle/min) | 16.4 ± 0.88 | 16.88 ± 0.88* |
| Heart rate (beat/min) | 85.36 ± 3.67 | 90.52 ± 3.50* |
| Systolic blood pressure (mmHg) | 117.47 ± 8.50 | 112.42 ± 8.71* |
| Diastolic blood pressure (mm Hg) | 66.63 ± 6.78 | 61.68 ± 6.46* |
| Body temperature (°C) | 37.05 ± 0.08 | 37.12 ± 0.094* |
Tab. 2. The vital signs before and after the administration of misoprostol.
The obstetrics history and examination revealed that the median gestation age was 10 weeks (assessed by the last menstrual period) or 8 weeks (assessed by ultrasonography) (Tab. 3.). Closed cervical oss was observed in 47 out of 95 cases (49.5%) and the minority presented with vaginal bleeding (9.5%).
| Findings | Frequency |
|---|---|
| Gestational age (week) | |
| Median (Range) | 10(8-12) |
| Last menstrual period | |
| Ultrasound | 8(5-11) |
| Cervical dilatation (cm) | |
| 0 | 33 |
| 0-1 | 38 |
| 1 | 17 |
| 2 | 7 |
| Vaginal bleeding | |
| No | 86 |
| Mild | 9 |
Tab. 3. Obstetrics assessment at the time of admission.
The total dosage of intra-vaginal tablets was not fixed for all patients. Tab. 4. showed the frequency–distribution of cases according to the total dosage of misoprostol. The majority of patients received either one dose (400 µg), two doses (800 µg), or three doses (1200 µg). The endpoint effects of misoprostol were observed in terms of cervical dilatation, vaginal bleeding, and the expulsion of gestation products (Tab. 4.). Complete expulsion of gestation product was observed in 38 out of 95 cases (40%) with different doses and times. 02 of admitted patients in this study required blood transfusion (2.1), and analgesia was prescribed to 27 patients (28.42%) in terms of Diclofenac sodium (11 cases), tramadol HCl (13 cases) and Meperidine HCl (3 cases). Prophylaxis antimicrobials were prescribed for all cases. The prophylactic use of antibiotics in the management of miscarriage is still controversial as many studies found the risk of infection to be low in all types of miscarriage management, However as our patients are not screened for genital tract infection we prefer to use prophylactic antibiotics for both surgical and medical evacuation to keep infection rates low. Misoprostol significantly induced changes in the vital signs (Tab. 2.). The respiratory rate, heart rate, and body temperature were significantly increased while systolic and diastolic blood pressures were reduced (Tab. 2.).
| Assessment | No. |
|---|---|
| Total misoprostol dose (µg) | |
| 400 | 24 |
| 800 | 25 |
| 1200 | 14 |
| 1600 | 12 |
| 2000 | 9 |
| 2400 | 11 |
| Cervical dilatation (cm) | |
| 0-1 | 25 |
| 1 | 13 |
| 01-02 | 39 |
| 2 | 28 |
| Vaginal bleeding | |
| Mild | 51 |
| Moderate | 40 |
| severe | 4 |
| Expulsion of gestation products | |
| Complete | 34 |
| Incomplete | 15 |
| Requirement of surgical abortion | 57 |
| Requirement of blood transfusion | 2 |
| Requirement of analgesia | |
| Diclofenac sodium | 11 |
| Tramadol HCl | 13 |
| Meperidine | 3 |
| Requirement of antimicrobials | 95 |
Tab. 4. The outcome and post medication follow up.
Tab. 5. summarized the adverse reactions of misoprostol. Abdominal pain (which was variable in severity) was reported in 19.98% and headache in 28.4% of cases, diarrhea in 2.10 of cases, fever in 1.05 of cases. Further analysis revealed that the prescribed dose is linked to several factors. Higher doses of misoprostol were required with higher gestational age groups (Tab. 6. and Fig. 1.) high discrepancy between gestational age by LMP and by US, high BMI, and older ages, interestingly the cervical dilatation was induced with misoprostol with any prescribed dose and the status of parity indirect influenced the recommended doses of misoprostol, and patients who had a previous history of the uterine scar required more doses of misoprostol (Tab. 6.).
| Adverse reaction | No. (%) |
|---|---|
| Hypersensitivity reaction | - |
| Fever (≥ 38°C) | 1 (1.05) |
| Headache | 27(28.42) |
| Diarrhea | 2 (2.10) |
| vomiting | 20(21.05) |
| Abdominal pain | |
| Mild | 9 (9.47) |
| Moderate | 7 (7.36) |
| Severe | 3(3.15) |
Tab. 5. Adverse reactions of intravaginal misoprostol.
| Administered dose | 400µg (n=24) |
800 µg (n=25) |
1200 µg (n=14) |
1600 µg (n=12) |
2000 µg (n=9) |
2400 µg (n=11) |
|---|---|---|---|---|---|---|
| Age (year) | 21.59 ± 5.7 | 24.85 ± 4.04 | 24.99 ± 9.9 | 30.10 ± 4.73 | 30.92 ± 3.86 | 28.75 ± 5.84 |
| BMI | 25.32 ± 2.65 | 23.12 ± 1.22 | 26.92 ± 2.95 | 27.82 ± 2.51 | 28.22 ± 2.76 | 28.32 ± 3.31 |
| Gest. age (week) | ||||||
| LMP | 10 ± 1.5 | 10.74 ± 1.09 | 10.6 ± 1.07 | 10.66 ± 1.5 | 11.0 ± 1.0 | 10.85 ± 1.3 |
| US | 9.33 ± 1.21 | 8.71 ± 1.25 | 8.7 ± 1.33 | 7.33 ± 1.59 | 7.94 ± 1.5 | 7.31 ± 1.43 |
| S. fibrinogen (mg/dl) | 331.29 ± 34 | 306.19 ± 28 | 283.80 ± 38 | 246.38 ± 26 | 203.25 ± 40 | 191.23 ± 44 |
| Cervical dilation (cm) | ||||||
| 0 | 1 | 5 | 5 | 8 | 7 | 7 |
| 0-1 | 17 | 12 | 3 | 2 | 3 | 1 |
| 1 | 8 | 7 | 1 | 0 | 0 | 1 |
| 2 | 2 | 1 | 1 | 2 | 1 | 0 |
| Parity | ||||||
| Null | 1 | 4 | 4 | 7 | 6 | 6 |
| Para 1 | 10 | 8 | 0 | 2 | 3 | 2 |
| Para 2 | 9 | 4 | 2 | 1 | 1 | 0 |
| Para 3 | 7 | 5 | 2 | 1 | 1 | 1 |
| Para 4 | 1 | 3 | 1 | 0 | 0 | 0 |
| Para 5 | 0 | 1 | 1 | 1 | 0 | 0 |
| Previous history of surgical abortion | 2 | 3 | 5 | 2 | 3 | 2 |
| Previous history of uterine scar | 0 | 1 | 2 | 2 | 1 | 2 |
Tab. 6. The recommended dose of misoprostol concerning the initial assessment.
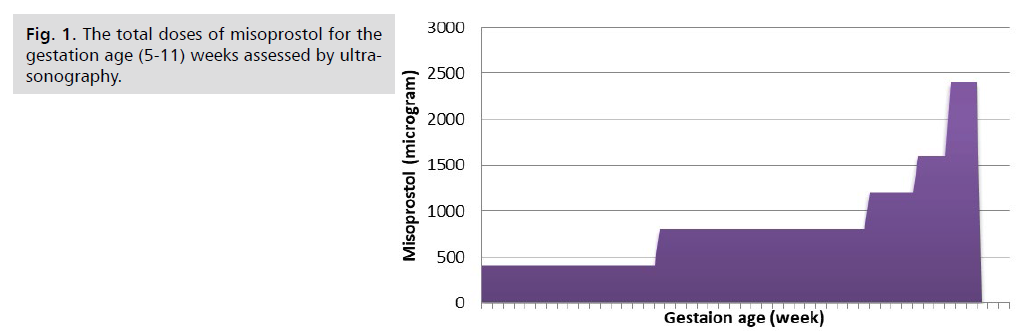
Fig 1. The total doses of misoprostol for the gestation age (5-11) weeks assessed by ultrasonography
Furthermore, the effects of misoprostol on the vital signs were well observed with multiple doses rather than with a single dose (Tab. 7.).
| Vital signs | 400µg (n=24) |
800 µg (n=25) |
1200 µg (n=14) |
1600 µg (n=12) |
2000 µg (n=9) |
2400 µg (n=11) |
|---|---|---|---|---|---|---|
| Resp. rate (cycle/min) | ||||||
| Before | 16.0 ± 0.58 | 16.0 ± 0.63 | 16.7 ± 0.82 | 16.54 ± 0.93 | 16.01 ± 70.61 | 16.33 ± 0.89 |
| After | 16.57 ± 0.53 | 16.33 ± 0.51 | 16.6 ± 0.7 | 17.18 ± 0.92** | 16.4 ± 0.3 | 16.84 ± 0.78** |
| Heart rate (beat /min) | ||||||
| Before | 81.7 ± 3.4 | 85.8 ± 3.2 | 85.4 ± 5.3 | 84.9 ± 1.95 | 83.8 ± 2.9 | 85.6 ± 3.8 |
| After | 85.0 ± 8.5 | 90.2 ± 2.6* | 91.4 ± 2.1** | 88.9 ± 1.95* | 87.6 ± 1.4 | 92.1 ± 2.4* |
| Systolic BP (mmHg) | ||||||
| Before | 120 ± 6.3 | 112.9 ± 4.1 | 119 ± 9.9 | 116.4 ± 7.8 | 125.7 ± 7.9 | 125.1 ± 8.6 |
| After | 115.0 ± 5.5 | 116.3 ± 8.7 | 112 ± 9.2* | 124.3 ± 5.3 | 112.6 ± 7.2** | 122.4 ± 9.3* |
| Diastolic BP ( mmHg) | ||||||
| Before | 71.0 ± 7.0 | 66.4 ± 3.8 | 67.0 ± 7.3 | 65.1 ± 6.4 | 68.3 ± 2.9 | 70.0 ± 6.3 |
| After | 67.0 ± 6.3 | 68.1 ± 4.9 | 60.6 ± 7.9* | 61.5 ± 5.4* | 63.4 ± 3.7 | 62.7 ± 4.1|*** |
| Temperature °C | ||||||
| Before | 37.12 ± 0.075 | 37.02 ± 0.048 | 37.04 ± 0.051 | 37.04 ± 0.094 | 37.19 ± 0.8 | 37.07 ± 0.076 |
| After | 37.23 ± 0.136 | 37.05 ± 0.053 | 37.06 ± 0.069 | 37.08 ± 0.075*** | 37.33 ± 0.211 | 37.2 ± 0.057* |
Tab. 7. Effect of misoprostol on vital signs of patients for the total dose of misoprostol.
Once again the adverse reactions of misoprostol were observed with high frequency when using multiple doses rather than with a single dose (Tab. 8.).
| Vital signs | 400µg (n=24) |
800 µg (n=25) |
1200 µg (n=14) |
1600 µg (n=12) |
2000 µg (n=9) |
2400 µg (n=11) |
|---|---|---|---|---|---|---|
| Abdominal pain | ||||||
| Mild | 1 | 1 | 2 | 1 | 1 | 3 |
| Moderate | 0 | 1 | 2 | 2 | 1 | 1 |
| Severe | 0 | 0 | 1 | 0 | 1 | 1 |
| Fever (≥38 °C) | 0 | 0 | 0 | 0 | 1 | 0 |
| Diarrhea | 0 | 0 | 0 | 0 | 1 | 1 |
| vomiting | 1 | 2 | 4 | 4 | 5 | 4 |
| Headache | 0 | 4 | 11 | 2 | 6 | 4 |
| Drug-induced hypersensitivity reaction | 0 | 0 | 0 | 0 | 0 | 0 |
Tab. 8. Systemic adverse reactions of misoprostol for the total dose.
Tab. 9. shows that vaginal bleeding as a sequence of the misoprostol Effect is observed in high frequency after administration of multiple doses compared with small doses.
| Outcomes | 400µg (n=24) |
800µg (n=25) |
1200µg (n=14) |
1600µg (n=12) |
2000µg (n=9) |
2400µg (n=11) |
|---|---|---|---|---|---|---|
| Vaginal bleeding | ||||||
| Mild | 22 | 18 | 6 | 3 | 1 | 1 |
| Moderate | 2 | 6 | 8 | 7 | 9 | 8 |
| Severe | 0 | 1 | 0 | 2 | 1 | 0 |
| Cervical dilatation | ||||||
| 0-1 | 0 | 1 | 2 | 3 | 4 | 5 |
| 1 | 1 | 1 | 1 | 3 | 3 | 4 |
| 1-2 | 13 | 12 | 5 | 5 | 4 | 0 |
| 2 | 10 | 11 | 6 | 1 | 0 | 0 |
| Requirement of analgesia | 2 | 4 | 8 | 5 | 3 | 5 |
| Complete expulsion of the gestational product | 1 | 6 | 8 | 7 | 8 | 4 |
| Add-on-surgical abortion | 23 | 19 | 5 | 3 | 3 | 4 |
| Successful medical abortion | 1 | 6 | 9 | 9 | 8 | 5 |
| Requirement of antimicrobials | 24 | 25 | 14 | 12 | 11 | 9 |
| In hospital stay (day) | ||||||
| 1 | 24 | 25 | 0 | 0 | 0 | 0 |
| 2 | 14 | 12 | 0 | 0 | ||
| 3 | 9 | 11 | ||||
Tab. 9. The outcome of using misoprostol for the dosage.
A higher degree of cervical dilatation was observed in high frequency with 1st three doses of misoprostol. The other data related to the complete expulsion of the gestation product, successful medication abortion, and requirement of analgesia, mainly accrued with multiple doses. Short day-stay in the hospital was also observed in high frequency with using a single dose of misoprostol.
Interestingly the results of this explored that successful medical abortion was observed in both primi-and multigravida without significant difference and medical abortion supplemented with surgical abortion did not offer advantages over medical abortion in primigravida or multigravida (Tab. 10.).
| Variables | Medical abortion | Medical supplemented with surgical abortion | Total |
|---|---|---|---|
| Primigravida | 11 (39.3%) | 17 (60.71%) | 28 |
| Multigravida | 27 (40.3%) | 40 (59.7%) | 67 |
| Total | 38 | 57 | 95 |
Tab. 10. Distribution of successful medical abortion versus medical abortion supplemented with surgical abortion for the parity.
The end response, as shown in Tab. 9. the patient's response was classified into 4 groups:
1. Complete expulsion of gestational products (34) 35.78%.
2. Partial expulsion of gestational products (17) 17.89%.
3. Add on surgical abortion (57) 60%.
4. Successful medical abortion (complete uterine evacuation without surgical intervention) (38) 40%.
Regarding successful medical abortion we can divide the patients into two groups as shown in Tab. 11.:
| Variables | Group(A) N=16 | Group(B) N=22 | P- value |
|---|---|---|---|
| Induction abortion interval (hrs) | 14.8 ± 6.08 | 29.72 ± 8.72 | 0 |
| Number of doses | 2.46 ± 1.08 | 4.95 ± 1.70 | 0 |
| Total dose (µg) | 998 ± 220 | 1981 ± 340 | 0 |
| Medical abortion within (18 hrs) | 16 (100%) | 0 (0%) | 0 |
| Successful medical abortion | 16 (42.10%) | 22 (57.89) | 0.03 |
| Mean age | 23,42 ± 2.20 | 28.56 ± 4.32 | 0.0001 |
| Body mass index | 25.382 ± 153 | 28.072 ± 2.42 | 0.002 |
| A discrepancy in gestational age (LMP/US) | 1.871 ± 1.23 | 3.267 ± 1.31 | 0 |
| Nulliparous women | 4(25%) | 7 (31.8%) | ------- |
| Multiparous women | 12(75%) | 15(68%) | ------- |
| Previous uterine scar | 3(37.5%) | 5(62.5%) | ˂ 0.05 |
Tab. 11. Comparison difference between two groups of Successful medical abortion.
1. Group (A): Those who received 3 doses or less of misoprostol (patients with criteria of best outcome).
2. Group (B): Those who received more than 3 doses of misoprostol.
The mean induction abortion interval was significantly shorter for group A than that for group B (14.8 ± 6.08 hrs, 29.72 ± 8.72) respectively with a p-value of 0.000 which is statistically significant.
It is also evident that all the ladies in group A were aborted within 1st 18 hrs compared with group B. with a p-value of 0.00 which is statistically significant.
The mean age was 23.42 ± 2.20 for group A and 28.56 ± 4.32 for group B with a p-value of 0.0001 which is statistically significant.
The mean BMI for group A was (25.382 ± 1.53), and (28.072 ± 2.42) for group B with a p-value of ˂0.0001 which is statistically significant.
Regarding the parity group A involved 25% of nulliparous women, and 75% of multiparous women, with a p-value of 0.005 which is statistically significant.
It is also shown that 3 (37%) of women with previous uterine scars were in group A, while 5(62%) were in group B.
The number of successful medical abortion were 16 (42%) for group A, while 22(62%) for group B.
Discussion
The medical management of early pregnancy failure seems to have a special impact on the health care of women of childbearing age in developing countries, where high-quality surgical care is not available to all. The World Health Organization estimates that globally one in every eight maternal deaths is due to abortion-related complications, hence the importance attached to this practice as a health problem [14].
Dilatation and Curettage which is one of the oldest procedures and one of the most frequently practiced operations is still risky in a small subset of patients. Possible complications include hemorrhage, PID, and perforation of the uterus.
The rate of uterine perforation in D/C is highest among women with missed abortions. Cameron IT, et al. [15]. So the need for the development of safer and more effective methods becomes the mandatory object.
Karim A [16] were the first to report on the successful use of PG in the management of intrauterine death, following this the use of PG for the management of missed abortion has been extensively researched in many trials where different types of PGs, both natural and synthetic has been used and currently PGs are the most widely used clinical method of termination.
Recently, two developments have led to further consideration being given to how to manage early pregnancy failure [17]: The first was technological advancements allowing a detailed examination of the uterine cavity with high-resolution transvaginal sonography for any retained products of conception. This technique can be used to identify the one in three women with a spontaneous abortion who do not retain significant amounts of tissue in the uterus, and consequently do not require any potentially damaging treatment. The second advancement was the development of misoprostol.
Misoprostol is often used alone or in combination with the progesterone receptor antagonist (mifepristone) to induce abortion. However, in early pregnancy failure antigestagens (mifepristone) are not necessary for medical termination of missed abortion as progesterone levels are usually low [17]. Our study regimen is (400 µg) intra-vaginal tablet of misoprostol every 6 hrs., for a maximum of three days, This regimen is proved by Bebbington MW, et al. trial [18] (The continuing administration of intravaginal misoprostol (400 µg) every 4-6 hrs., for a maximum period of 3 days has recently been shown to be effective in first-trimester spontaneous abortion).
According to our data in the results, the total dosage of intra-vaginal misoprostol tablet was not fixed for all patients. Higher doses of misoprostol were required with an increase in the gestational age (by LMP), this is disagree with Zhang J, et al. [19] (Pregnancy duration did not affect the rate of successful expulsion), and agree with Spitz IM, et al. [20] and Allen RH, et al. [21] and Several studies suggest the success rate of medical abortion to be dependent on the duration of gestation.
Also, Higher doses of misoprostol were required when there is a high discrepancy between gestational age by LMP and by US (old missed), this is agree with Creinin et al. (the longer fetal death period, the less estrogen level in the blood, and the uterus become less sensitive to the effect of oxytocic drugs as well as to prostaglandin receptors through a direct effect on their chemical configuration) [22]. Women with higher BMI were required more doses of misoprostol, in form of low BMI women responded better to misoprostol than overweight and obese women.
The status of parity is indirectly influenced by the recommended doses of misoprostol. High parity responded better to 1st-trimester abortion induced by misoprostol, this is agreed with Bugalho A, et al. [23] (in his study: women with high parity responded better to 1st-trimester abortion induced by misoprostol), This is because Misoprostol like other uterotonic agents is more effective in multiparous than in nulliparous women, may be due to increasing the sensitivity of the uterus to uterotonic agents as parity increase.
But disagree with Ashok PW, et al. [24], and Bartley J, et al. [25] in their studies (parous women have had lower complete abortion rates after medical abortion compared with nulliparous women).
Also, the age factor in form of younger women is a better response to misoprostol. This also agrees with Bugalho A, et al. [23] (younger women responded better to 1st-trimester abortion induced by misoprostol).
Interestingly patients who had a previous history of the uterine scar required more doses of misoprostol. These findings are inconsistent with the result obtained by Beatrice A, and Kurt Barnhart (who found that in women with previous uterine surgery, vaginal misoprostol treatment for early pregnancy failure resulted in similar rates of success, acceptability, and adverse events compared with women without previous uterine surgery. There was no difference in the acceptability of side effects of Misoprostol for treatment of early pregnancy failure in women with previous uterine surgery) [26,27]. Also, women with higher serum fibrinogen level respond better to misoprostol which in turn they depend indirectly on the estrogen level circulating in the blood. Once missed abortion occurs, the placenta dies also and the fraction of circulating estrogen contributed by the placenta is removed. In addition, the release of tissue thromboplastin occurs continuously from the dead placenta leading ultimately to the depletion of the clotting factors and fibrinogen level [27].
Other results show that a short day stay in the hospital was observed in high frequency with using a single dose of 400 µg.
Once again the adverse reactions of misoprostol and the requirement of analgesia were observed in high frequency with multiple doses, rather than with a single dose (400µg), this may be due to the prolonged or sustained effect of misoprostol. Only two cases were reported of fever which resolved spontaneously 2nd the day, this is not agreed with Bebbington (there was an increase in febrile morbidity in the vaginal misoprostol) [18].
Another notable side effect was abdominal pain which was observed in 23 patients and required opioid analgesia.
The rest of the side effects are non-eventful and resolved spontaneously without treatment such as headache, nausea, vomiting, & diarrhea with or without abdominal pain and cramps (due to the stimulation of gastrointestinal motility).
Ayres D, et al. [28] and Graziosi GC, et al. [29] have shown that it is cheaper to manage early pregnancy failure with misoprostol than surgical intervention and that women prefer this method, it seems likely that misoprostol treatment will become a standard or preferred treatment for early pregnancy failure.
Conclusion
Younger age, low BMI, multi parity, initial cervical dilatation, short time fetal death as well as absent previous history of uterine scar, all are the criteria of the patient with the best outcome when using misoprostol vaginally for 1st trimester missed abortion and can be a reliable predictor to uterine response for vaginal misoprostol when used for 1st trimester missed abortion. Intra-vaginal misoprostol alone as monotherapy at a dose of 400 µg every 6 hours is an effective regimen to achieve successful termination of 1st trimester missed abortion. Moistening of misoprostol by normal saline is more effective than dry misoprostol. 2nd and 3rd dose effectiveness of misoprostol was observed. The adverse effects of misoprostol are minimal and dose-related and self-limiting.
References
- Rai R, Regan L. Recurrent miscarriage. The lancet. 2006;368(9535):601-611.
- Regan L, Braude PR, Trembath PL. Influence of past reproductive performance on risk of spontaneous abortion. Br Med J. 1989;299(6698):541-545.
- Royal College of Obstetricians and Gynecologists. No Gt. The Management of Early Pregnancy Loss. Management. 2006;1:2.
- Alberman E. Spontaneous abortions: epidemiology. Spontaneous Abort. 1992:9-20.
- Norman JE, Thong KJ, Baird DT. Uterine contractility and induction of abortion in early pregnancy by misoprostol and mifepristone. The lancet. 1991;338(8777):1233-1236.
- Miriani Neto C, Delbin AL, Val Júnior RD. Padräo tocográfico desencadeado pelo misoprostol. Rev Paul Med. 1988:205-208.
- Aubeny E, Baulieu EE. Activité contragestive de l'association au RU486 d'une prostaglandine active par voie orale. Comptes rendus de l'Académie des sciences. Serie III: Sciences de la Vie. 1991;312(11):539-545.
- El-Refaey H, Templeton A. Early induction of abortion by a combination of oral mifepristone and misoprostol administered by the vaginal route. Contraception. 1994;49(2):111-114.
- Alfirevic Z, Howarth G, Gaussmann A. Selected Cochrane Systematic Reviews: Oral Misoprostol for Induction of Labour with a Viable Fetus. Birth. 2000;27(4):286-.
- Hofmeyr GJ, Milos D, Nikodem VC, et al. Limb reduction anomaly after failed misoprostol abortion. S Afr Med J.1998;88(5):566.
- Davies NM, Longstreth J, Jamali F. Misoprostol therapeutics revisited. Pharmacotherapy. 2001;21(1):60-73.
- Schong YS, Chua S, Arulkumaran S. Severe hyperthermia following oral misoprostol in the immediate postpartum period. Obstet Gynecol. 1997;90(4 Part 2):703-704.
- Goldberg AB, Greenberg MB, Darney PD. Misoprostol and pregnancy. N Engl J Med. 2001;344(1):38-47.
- WHO U. UNFPA.(2004). Maternal mortality in 2000: Estimates developed by WHO, UNICEF, UNFPA. 2000.
- Cameron IT, Michie AF, Baird DT. Therapeutic abortion in early pregnancy with antiprogestogen RU486 alone or in combination with prostaglandin analogue (gemeprost). Contraception. 1986;34(5):459-468.
- Karim A. Antiulcer prostaglandin misoprostol: single and multiple dose pharmacokinetic profile. Prostaglandins. 1987;33:40-50.
- Winikoff B. Pregnancy failure and misoprostol-time for a change. N Engl J Med. 2005;353(8):834-836.
- Bebbington MW, Kent N, Lim K, et al. A randomized controlled trial comparing two protocols for the use of misoprostol in midtrimester pregnancy termination. Am J Obstet Gynecol. 2002;187(4):853-857.
- Zhang J, Gilles JM, Barnhart K, et al. A comparison of medical management with misoprostol and surgical management for early pregnancy failure. N Engl J Med. 2005;353(8):761-769.
- Spitz IM, Bardin CW, Benton L, et al. Early pregnancy termination with mifepristone and misoprostol in the United States. N Engl J Med. 1998;338(18):1241-1247.
- Allen RH, Goldberg AB. Cervical dilation before first-trimester surgical abortion (< 14 weeks' gestation). SFP Guideline 20071. Contraception. 2007;76(2):139-156.
- Creinin MD, Vittinghoff E, Keder L, et al. Methotrexate and misoprostol for early abortion: a multicenter trial. I. Safety and efficacy. Contraception. 1996;53(6):321-327.
- Bugalho A, Faundes A, Jamisse L, et al. Evaluation of the effectiveness of vaginal misoprostol to induce first trimester abortion. Contraception. 1996;53(4):243-246.
- Ashok PW, Templeton A, Wagaarachchi PT, et al. Factors affecting the outcome of early medical abortion: a review of 4132 consecutive cases. BJOG: Int J Obstet Gynaecol. 2002;109(11):1281-1289.
- Bartley J, Tong S, Everington D, et al. Parity is a major determinant of success rate in medical abortion: a retrospective analysis of 3161 consecutive cases of early medical abortion treated with reduced doses of mifepristone and vaginal gemeprost. Contraception. 2000;62(6):297-303.
- Hausknecht RU. Methotrexate and misoprostol to terminate early pregnancy. N Engl J Med. 1995;333(9):537-540.
- Creinin MD, Vittinghoff E, Keder L, et al. Methotrexate and misoprostol for early abortion: a multicenter trial. I. Safety and efficacy. Contraception. 1996;53(6):321-327.
- Ayres-de-Campos D, Teixeira-da-Silva J, Campos I, et al. Vaginal misoprostol in the management of first-trimester missed abortions. Int J Gynaecol Obstet. 2000;71(1):53-57.
- Graziosi GC, Van der Steeg JW, Reuwer PH, et al. Economic evaluation of misoprostol in the treatment of early pregnancy failure compared to curettage after an expectant management. Hum Reprod. 2005;20(4):1067-1071.
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Author Info
Hameed Jameel Hamzah1, Russul Daad Abd Oun1, Tahsin Hadi Husain1, Akhlas Hashem Salman1* and Al-Sharifi AZ22Department of Gynecology and Obstetrics, College of Medicine, Al-Mustansyria University, Baghdad, Iraq
Copyright:This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.