Research Article - (2022) Volume 17, Issue 2
Comparison between abdominal sacral hysteropexy and vaginal sacrospinous hysteropexy for management of women with apical uterine descent : A randomized clinical trial
Ihab Gomaa, Mohammad NasrAl Deen, Tamer Farouk Borg, Mahmoud Ghaleb, Asmaa Ragab* and Basem Aly IslamReceived: 25-Mar-2022, Manuscript No. gpmp-22-58563; Editor assigned: 26-Mar-2022, Pre QC No. P-58563; Reviewed: 30-Mar-2022, QC No. Q-58563; Revised: 04-Apr-2022, Manuscript No. R-58563; Published: 29-Jun-2022
Abstract
Aim: Regarding surgical treatment of uterine prolapse, sacral colpopexy has been reported to show low risk of recurrence. Previous studies paid less attention to functional outcomes, peri-operative problems and surgical lengths of stay. We here attempted to determine which is clinically better, abdominal sacral hysteropexy (ASH) vs. vaginal sacrospinous hysteropexy (SSF) in women with apical prolapse.
Methods: Patients consisted of 72 women with apical uterine descent stage II or more according to POP-Q, who were treated in Ain Shams University Maternity Hospital. These patients were randomly divided into two groups; ASH (n=37) vs. SSF (35). Operative time, peri-operative complications, and length of stay were compared. Follow up visits at 4 weeks, 3 months, 6 months and 1 year were scheduled. We assessed recurrent or de novo prolapse, urinary incontinence, need for re- operation, the sexual function, and the quality of life.
Results: The two groups showed similar background. ASH, compared with SSF, showed the followings; 1) less frequent recurrence, 2) less frequent re-surgery at 1 year, 3) less frequent presence of symptoms at 1 year, 4) longer operative time, more blood loss, and longer hospital stay, 4) more frequent minor complications.
Conclusion: ASH, compared with SSF, showed a lower rate of recurrence, but with significantly larger amount of intra-operative blood loss, postoperative pyrexia, and hospital stay. We must consider this merit/demerit of ASH when we choose the procedure.
Keywords
Abdominal sacral hysteropexy; Recurrent uterine prolapse; Sacrospinous ligament fixation.
Introduction
Women's quality of life (QoL) is negatively impacted by Pelvic organ prolapse (POP), a frequent gynecological issue that limits a woman's ability to engage in physical, social, and sexual activities. Prolapse or incontinence surgery has a lifetime risk of between 11% and 19%, according to epidemiological research, and up to a third of these patients need further treatment for recurrence [1].
The frequency of these procedures is predicted to rise with an ageing population, despite the fact that rising rates of cesarean sections and decreasing family sizes in recent years will have a negative influence on their prevalence. In multiparous women over 50, prolapse of the pelvic organs is quite prevalent (affects approximately 50 percent of women over age 50). Patients' self-perceptions of their bodies and sexuality may be harmed by pelvic organ prolapse [2].
While there are various ways to fix POP surgically, the surgeon must ultimately select whether to execute this treatment by open or laparoscopic means, depending on what kind of POP it is and where it is located. Additional judgments must be made on whether synthetic or biological grafts will be used to support the repair [3].
This study aimed to evaluate the operative time, effectiveness and safety of vaginal sacrospinous hysteropexy and abdominal sacral hysteropexy.
Patients and Methods
The study was conducted at the Urogynaecology unit, Ain Shams University Maternity Hospital on 72 women with symptomatic apical uterine descent stage II or more according to (POP-Q) that started in June 2020 and ended in March 2022. Each group initially included 37 patients. Two patients from the SSF group were excluded from the analysis, 1 of them withdrew from the study and the other was lost to follow up. The study protocol was approved by Research Ethics Committee of the council of Obstetrics and Gynecology Department, Ain Shams University. Also informed written consent after explaining the study purpose and method to the subjects was taken. Women were randomly allocated into two groups; 37 patients in ASH group included and 35 patients in SSF group that were performed by a senior urogynecologist.
Patients were included in the study if presented with symptomatic apical prolapse stage II or more according to POP-Q after exclusion of any uterine or cervical pathology. The exclusion criteria were:
1. Women with contraindication for any operations
2. Women with recurrent apical prolapse surgery
3. Non feasibility of any of the two procedures
4. Women who preferred to have hysterectomy
Detailed history, Physical examination including POP-Q and preoperative investigation were done. The primary outcome was the operative time, and the secondary outcomes were the recurrence rate, the adverse events as blood loss, bladder or bowel injury, wound infection and post-operative pyrexia, hospital stay and effect on quality of life and sexual function.
Randomization
Randomization was carried out by the coordinating researcher centrally through a website utilizing a computer- generated randomization table once patients had given their permission to participate in the trial. The vaginal and abdominal approaches were given to the test individuals in a 1:1 ratio. The information was kept private. After randomization, those who opted out of the study were treated according to the patient's request.
Allocation and concealment
SNOSE (serially numbered opaque sealed envelopes) was used to conceal the group until allocation and in each envelope the corresponding letter which denotes the allocated group (ASH group or SSF group) were put according to randomization plan. Then all envelopes were closed and put in one box. When the first patient arrived, the first envelope was opened, and the patient was allocated according to the letter inside.
Sample size and justification
Using PASS "program for sample size calculation [4], the expected mean-operation time in the study groups = 90 ± 20 minutes for the abdominal group and 56 ± 11.67 min. for the vaginal group, setting power at 90% and α-error at 0.05, sample size of 35 women per group is enough.
Procedures
Abdominal sacral hysteropexy: After anesthesia, the patient was placed in semi-lithotomy position. The abdomen was entered via a transverse incision. After identification of the right ureter and the left common iliac vein, a longitudinal incision was made over the anterior surface of sacral promontory to expose the anterior longitudinal ligament. The incision extended downward till the level of uterosacral ligaments. Fixation of a macroporus polypropylene mesh 15*3 cm to the back of uterine cervix using 3 rows of 6 transverse-interrupted 2-0 Polypropylene sutures, then the mesh was attached to the anterior longitudinal ligament overlying the sacral promontory after adjustment the length using 3 transverse-interrupted 2-0 Polypropylene sutures about ½ cm apart, without being too tight, to help maintain a horizontal rather than an upright direction of the upper vagina on standing, then removal of excess mesh. The incised parietal peritoneum was sutured with (polyglactin 910, 2/0).
Vaginal sacrospinous hysteropexy: Woman was placed in lithotomy position. The pararectal space was used to gain entry to the sacrospinous ligament. An incision was made in the perineum and the posterior vaginal wall. The rectum was taken away from the posterior vaginal wall. The right ischial spine was localized digitally and after breisky retractor positioning, one superiorly to retract the urinary bladder, one medially to retract the rectum and one laterally to retract the pubococcygeal muscle, the ligament was made visible through blunt dissection of the right rectal pillars. At least 2 cm from the ischial spine, two permanent sutures were inserted under direct vision through the right sacrospinous ligament, one at least 1 cm apart and medially (Polypropylene 1.0, Ethicon Inc., Sommerville, NJ, USA). Additional posterior-colporrhaphy was performed. Dissection of the supravaginal portion of the cervix. The sutures were inserted through the posterior side of the cervix and two thirds of the posterior vaginal wall was closed with (Polyglactin 910, 2.0). The cervix was redressed after the sutures were tightened. The remaining portion of the vaginal wall was sutured.
Operative time was calculated using stop watch from the moment of the surgical skin or vaginal incision till its closure, also time of hysteropexy only was recorded. Blood loss was calculated using aspirated blood and visual estimation of common surgical gauze. Any intra- operative complications were recorded. One of the research team followed the patients all through their hospital stay till discharge. All patients were asked for return visits at 1 month, 3 months, 6 months and 1year post-operative for follow up. Every time a patient came in, the POP-Q system was used to gather information about their medical history and assess their clinical efficacy. Prolapse-quality of life questionnaire (P-QOL) and prolapse/urinary incontinence/sexual function questionnaire was used to evaluate the impact on quality of life and sexual function, respectively (PISQ-12).
Statistical analysis
The statistical program for social sciences (SPSS) version 23.0 was used to evaluate the recorded data (SPSS Inc., Chicago, Illinois, USA). A mean, standard deviation, or median with an inter-quartile range was used to represent the quantitative data (IQR). Qualitative factors were also shown in percentages and numbers. Kolmo-gorov-Smirnov and Shapiro-Wilk tests were used to examine the data for normality. Independent-samples t-test or Mann Whitney U test was used to compare between groups regarding numeric variables. Chi-squared test was used to compare both groups regarding categorical variables. Multivariate logistic regression analysis with odds ratios (OR) and 95% confidence intervals to assess the overall association between each possible risk factor and the occurrence of (recurrent uterine descent, de novo cystocele, de novo rectocele and need another surgery), and Kaplan-Meier Survival Analysis which is a descriptive procedure for examining the distribution of time-to-event variables.
Results
Although subjective assessment was not statistically significant till 6 months post-operative, there was statistically significant difference according to patient’s symptoms at 1 year post-operative. The higher number of symptomatic patients were in SSF group 16 patients (45.7%) compared with ASH group 8 patients (21.6%), these symptoms included awareness of prolapse, urinary and sexual symptoms as a total, but there was no statistically significant difference between both groups as regard presence of urinary incontinence, sexual function and quality of life at 1 year (Tab. 1- 4).
| Demographic data | ASH | SSF | Test value | p-value |
|---|---|---|---|---|
| Age (years) (Mean ± SD) | 39.22 ± 8.11 | 43.20 ± 4.96 | t=1.572 | 0.120 |
| BMI [kg/m2] (Mean ± SD) | 34.20 ± 5.92 | 33.22 ± 4.45 | t=0.79 | 0.432 |
| Parity (Median) (IQR) | 3 (3-4) | 4 (3-5) | U=-1.836 | 0.071 |
| Diabetes Mellitus | 1 (2.7%) | 3 (8.6%) | χ2=1.174 | 0.279 |
| Hypertension | 3 (8.1%) | 5 (14.3%) | χ2=0.690 | 0.406 |
| Menopause | 6 (16.2%) | 14 (40%) | χ2=5.071 | 0.024* |
| Bronchial asthma | 8 (21.6%) | 6 (17.1%)) | χ2=0.034 | 0.854 |
| Chronic constipation | 2 (5.4%) | 1 (2.9%) | χ2=0.004 | 0.953 |
| More than one risk factor | 35 (94.6%) | 35 (100%) | χ2=2.747 | 0.097 |
| Surgical history | ||||
| Classical repair | 2 (5.4%) | 1 (2.9%) | χ2=0.276 | 0.599 |
| Transe obturator tape (TOT) | 2 (5.4%) | 0 (0.0%) | χ2=1.917 | 0.166 |
| Tension free vaginal tape (TVT) | 0 (0.0%) | 1 (2.9%) | χ2=1.073 | 0.300 |
| Urinary symptoms | ||||
| Stress urinary incontinence (SUI) | 11 (29.7%) | 9 (25.7%) | χ2=0.142 | 0.707 |
| Over active bladder (OAB) | 7 (18.9%) | 6 (17.1%) | χ2=0.039 | 0.844 |
| Voiding dysfunction | 0 (0.0%) | 2 (5.7%) | χ2=0.125 | 0.723 |
| Preoperative stage of uterine descent | ||||
| II | 25 (67.6%) | 24 (68.6%) | χ2=2.395 | 0.302 |
| III | 12 (32.4%) | 9 (25.7%) | χ2=0.386 | 0.535 |
| IV | 0 (0.0%) | 2 (5.7%) | χ2=2.139 | 0.144 |
Tab. 1. Comparison between ASH group and SSF group according to demographic data.
| Peri-operative data | ASH (n=37) | SSF (n=35) | Test value | p-value |
|---|---|---|---|---|
| Concomitant surgeries | ||||
| Posterior colporrhaphy +\- perineorrhaphy | 5 (13.5%) | 8 (22.9%) | - | - |
| Anterior colporrhaphy | 1 (2.7%) | 3 (8.6%) | - | - |
| Burch colposuspention | 9 (24.3%) | 0 (0.0%) | - | - |
| Moschowitz | 1 (2.7%) | 0 (0.0%) | - | - |
| Paravaginal repair | 1 (2.7%) | 0 (0.0%) | - | - |
| Transe obturator tape (TOT) | 2 (5.4%) | 12 (34.3%) | - | - |
| Tension free vaginal tape (TVT) | 2 (5.4%) | 1 (2.9%) | - | - |
| Operative Time of hystropeχy (min) (Mean ± SD) | 95.65 ± 13.73 | 35.40 ± 9.88 | U=21.263 | <0.001** |
| Blood loss (ml) (Mean ± SD) | 551.35 ± 161.08 | 292.71 ± 51.57 | U=9.067 | <0.001** |
| Blood Transfusion | 6 (16.2%) | 1 (2.9%) | χ2=3.657 | 0.056 |
| Bladder injury | 2 (5.4%) | 0 (0.0%) | χ2=1.917 | 0.166 |
| Pudendal nerve injury (Buttock pain) | 0 (0.0%) | 2 (5.7%) | χ2=2.139 | 0.144 |
| rectal injury | 0 (0.0%) | 1 (2.9%) | χ2=1.073 | 0.300 |
| Wound infection | 6 (16.2%) | 1 (2.9%) | χ2=3.657 | 0.056 |
| Pyreχia | 19 (51.4%) | 11 (31.4%) | χ2=2.937 | 0.087 |
| Hospital stay (days) (Mean ± SD) | 5.78 ± 2.57 | 2.86 ± 0.94 | U=6.337 | <0.001** |
| PISQ-12 score at 1 year (Mean ± SD) | 37.01 ± 2.91 | 38.09 ± 4.13 | t=1.193 | 0.238 |
| P-QOL score at 1 year ( Mean ± SD) | 106.54 ± 22.92 | 114.51 ± 32.96 | U=1.431 | 0.236 |
| De novo incontinence at 1 year | ||||
| De novo stress urinary incontinence (SUI) | 4 (10.8%) | 4 (11.4%) | χ2=0.007 | 0.934 |
| De novo urge | 6 (16.2% | 1 (2.9%) | χ2=3.657 | 0.056 |
Tab. 2. Comparison between ASH and SSF according to intraoperative and postoperative data.
| Subjective assessment | At 1 month | At 3 months | At 6 months | At 12 months | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ASH (n=37) | SSF (n=35) | χ2 | p-value | ASH (n=37) | SSF (n=35) | χ2 | p-value | ASH (n=37) | SSF (n=35) | χ2 | p-value | ASH (n=37) | SSF (n=35) | χ2 | p-value | |
| Symptomatic patients | 0 (0.0%) | 0 (0.0%) | 0.000 | 1.000 | 0 (0.0%) | 3 (8.6%) | 3.309 | 0.069 | 3 (8.1%) | 5 (14.3%) | 0.695 | 0.404 | 8 (21.6%) | 16 (45.7%) |
4.698 | 0.030* |
Tab. 3. Comparison between Group A: ASH and Group B: SSF according to bothersome symptoms.
| Objective assessment | At 1 month | At 3 months | At 6 months | At 6 months | At 12 months | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ASH (n=37) | SSF (n=35) | χ2 | p-value | ASH (n=37) | SSF (n=35) | χ2 | p-value | ASH (n=37) | SSF (n=35) | χ2 | p-value | ASH (n=37) | SSF (n=35) | χ2 | p-value | ASH (n=37) | SSF (n=35) | χ2 | p-value | |
| Recurrent Ut. prolapse = C3-1 | 0 (0.0%) | 0 (0.0%) | NA | NA | 0 (0.0%) | 0 (0.0%) | NA | NA | 1 (2.7%) | 2 (5.7%) | 0.409 | 0.523 | 1 (2.7%) | 2 (5.7%) | 0.409 | 0.523 | 2 (5.4%) | 7 (20.0%) | 3.503 | 0.061 |
| De novo Cystocele = Aa3-1 |
0 (0.0%) | 0 (0.0%) | NA | NA | 0 (0.0%) | 3 (8.6%) | 3.275 | 0.070 | 2 (5.4%) | 3 (8.6%) | 0.279 | 0.597 | 2 (5.4%) | 3 (8.6%) | 0.279 | 0.597 | 4 (10.8%) | 9 (25.7%) | 2.700 | 0.100 |
| De novo Rectocele = Ap3-1 |
0 (0.0%) | 0 (0.0%) | NA | NA | 0 (0.0%) | 0 (0.0%) | NA | NA | 1 (2.7%) | 1 (2.9%) | 0.003 | 0.959 | 1 (2.7%) | 1 (2.9%) | 0.003 | 0.959 | 4 (10.8%) | 3 (8.6%) | 0.103 | 0.749 |
| Need another surgery | 0 (0.0%) | 0 (0.0%) | NA | NA | 0 (0.0%) | 3 (8.6%) | 3.309 | 0.069 | 4 (10.8%) | 5 (14.3%) | 0.199 | 0.656 | 4 (10.8%) | 5 (14.3%) | 0.199 | 0.656 | 8 (21.6%) | 16 (45.7%) |
4.698 | 0.030* |
Tab. 4. Comparison between Group A: ASH and Group B: SSF according to objective assessment using POP-Q.
Fig. 1. Kaplan-Meier survival curves between Group A: ASH and Group B: SSF. There was statistically significant difference among the 2 survival curves (Log-rank chi- squared = 4.717, df = 1, p-value = 0.030*), indicating that the time to be symptomatic for POP after surgery was significantly shorter in the SSF group, Symptoms of POP started at 3 months in SSF group and at 6 months in ASH group. 3 patients started to develop symptoms of POP at 6 months post-operative and another 5 patients at 1 year post- operative in ASH group to have 8 patients as a total that became symptomatic for POP at 1 year. 3 patients started to develop symptoms of POP at 3 months post-operative, another 2 patients at 6 months post-operative and another 11 patients at 1 year post-operative in SSF group to have 16 patients as a total that became symptomatic for POP at 1 year. The higher number of symptomatic patients was at 1 year and in SSF group.
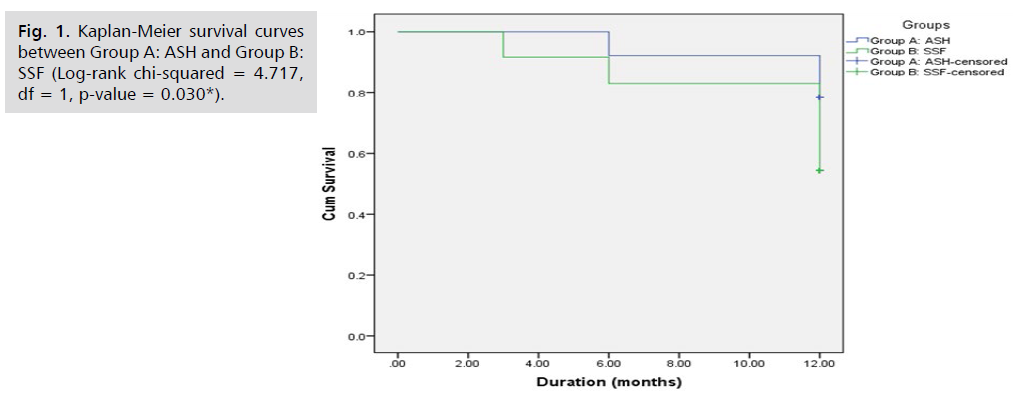
Fig 1: Kaplan-Meier survival curves between Group A: ASH and Group B: SSF (Log-rank chi-squared = 4.717, df = 1, p-value = 0.030*).
Fig. 2. Kaplan-Meier survival curves between ASH and SSF groups. There was no statistically significant difference among the 2 survival curves (Log-rank chi-squared = 3.375, df = 1, p-value = 0.066), indicating that the time to surgical failure (recurrent uterine prolapse) was insignificant in both groups. Recurrence of uterine prolapse started at 6 months in both groups. It started in one patient at 6 months post- operative and in another patient at 1 year post-operative in ASH group to have recurrent uterine prolapse in 2 patients as a total along 1 year. Recurrence of uterine prolapse started in 2 patients at 6 months post-operative and in another 5 patients at 1 year post-operative in SSF group to have recurrent uterine prolapse in 7 patients as a total along 1 year. The higher number of recurrence occurred in SSF group at 1 year.
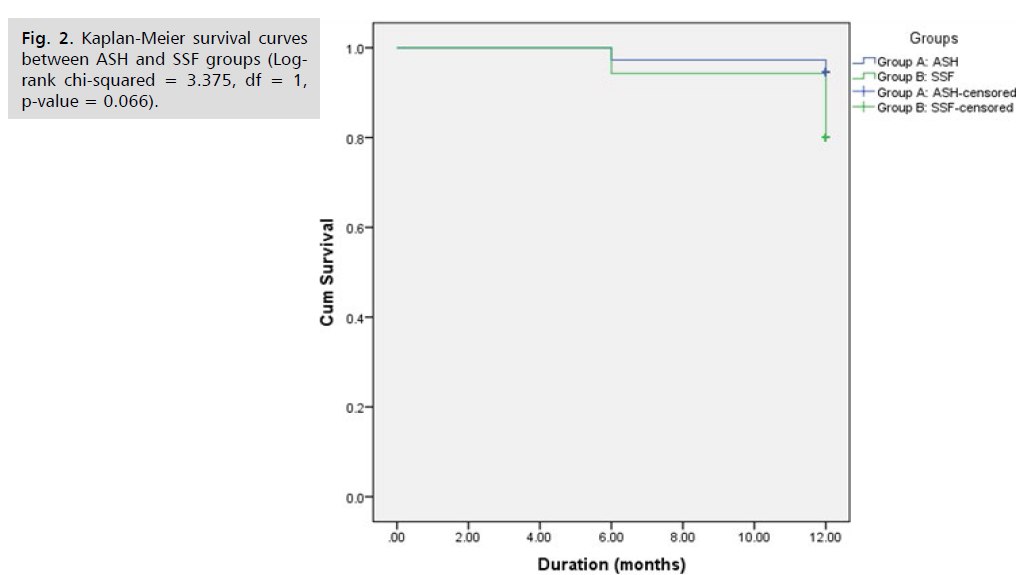
Fig 2: Kaplan-Meier survival curves between ASH and SSF groups (Logrank chi-squared = 3.375, df = 1, p-value = 0.066).
Fig. 3. Kaplan-Meier survival curves between Group A: ASH and Group B: SSF. There was no statistically significant difference among the 2 survival curves (Log- rank chi-squared = 2.374, df = 1, p-value = 0.123). De novo cystocele started in 2 patients at 6 months post-operative and in another 2 patients at 1 year post-operative in ASH group to have De novo cystocele in 4 patients as a total along 1 year. De novo cystocele started in 3 patients at 3 months post-operative and in another 6 patients at 1 year post-operative in SSF group to have De novo cystocele in 9 patients as a total along 1 year. De novo cystocele started to occur after 6 months in ASH group and after 3 months in SSF group. The higher rate of De novo cystocele was in SSF group 1 year post-operative.
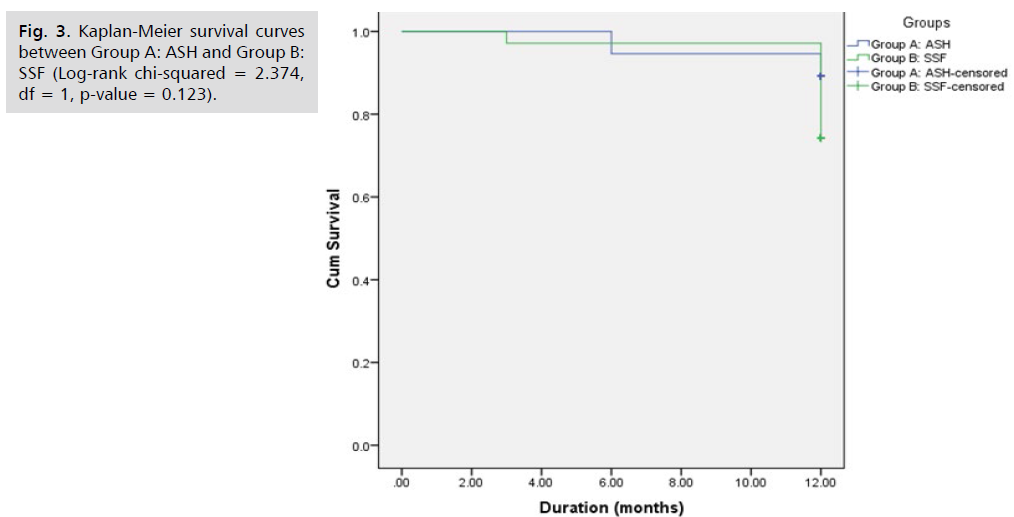
Fig 3: Kaplan-Meier survival curves between Group A: ASH and Group B: SSF (Log-rank chi-squared = 2.374, df = 1, p-value = 0.123).
Fig. 4. Kaplan-Meier survival curves between Group A: ASH and Group B: SSF. There was no statistically significant difference among the 2 survival curves (Log- rank chi-squared = 0.096, df = 1, p-value = 0.756). De novo rectocele started in one patient at 6 months post-operative and in another 3 patients at 1 year post-operative in ASH group to have De novo rectocele in 4 patients as a total along 1 year. De novo rectocele started in one patient at 6 months post-operative and in another 2 patients at 1 year post-operative in SSF group to have De novo rectocele in 3 patients as a total along 1 year. De novo rectocele started to occur 6 months postoperative in both groups. The higher rate of De novo rectocele was in ASH group 1 year post- operative.
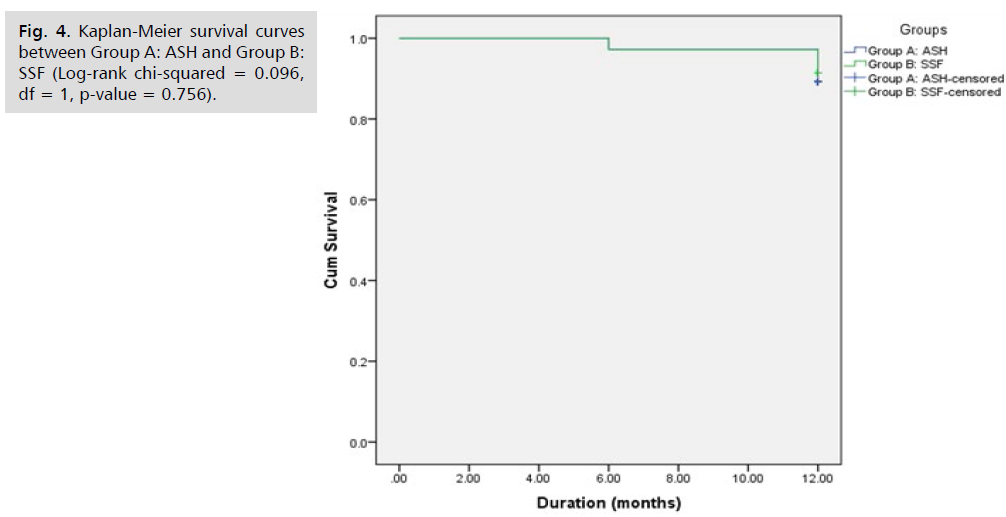
Fig 4: Kaplan-Meier survival curves between Group A: ASH and Group B: SSF (Log-rank chi-squared = 0.096, df = 1, p-value = 0.756).
Fig. 5. Kaplan-Meier survival curves between ASH and SSF groups. There was statistically significant difference among the 2 survival curves (Log-rank chi-squared = 3.780, df = 1, p-value = 0.042*), indicating that the time to re- operation was significantly shorter in the SSF group there were 4 patients needed another surgery at 6 months post- operative and another 4 patients at 1 year post-operative in ASH group to have 8 patients (21.6%) as a total that needed another surgery either for uterine and vaginal prolapse or anti-incontinence surgery at 1 year. There were 3 patients needed another surgery at 3 months post- operative, another 2 patients at 6 months post-operative and another 11 patients at 1 year post-operative in SSF group to have 16 patients(45.7%) as a total that need another surgery either for uterine or vaginal prolapse repair at 1 year. The higher number of patients needed another surgery either for uterine or vaginal prolapse surgery was significant in SSF group at 1 year post-operative.
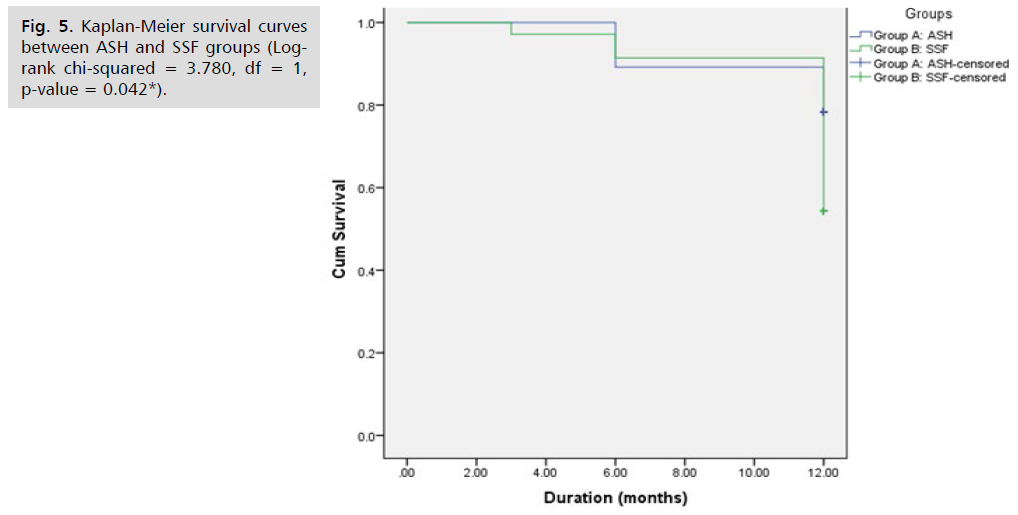
Fig 5: Kaplan-Meier survival curves between ASH and SSF groups (Logrank chi-squared = 3.780, df = 1, p-value = 0.042*).
This Tab. 5. showed that Age (years), multiple risk factors >2 risk, Type of surgery (SSF<ASH), Pre Stage of uterine descent and Menopausal state, had a significant positive correlation with the rate of recurrence of uterine prolapse, with p-value (p<0.05).
| Parameters | β | S.E. | Sig. | Odds Ratio | C.I. 95% | |
|---|---|---|---|---|---|---|
| Lower | Upper | |||||
| Age (years) | -3.25 | 0.97 | <0.001** | 0.04 | 0.01 | 0.26 |
| Multple risk factors >2 risk | 1.24 | 0.55 | 0.024* | 3.45 | 1.18 | 10.09 |
| Type of surgery | 3.46 | 0.99 | <0.001** | 31.66 | 4.56 | 220.07 |
| Pre Stage of ut. Descent | 1.17 | 0.47 | 0.014* | 3.23 | 1.27 | 8.19 |
| Time of hystropeχy (min) | -0.23 | 0.49 | 0.638 | 0.79 | 0.30 | 2.07 |
| Intraoperative complications | 0.66 | 0.40 | 0.098 | 1.94 | 0.89 | 4.24 |
| Menopausal state | 3.52 | 0.80 | <0.001** | 33.72 | 7.06 | 161.07 |
| Constant | -12.18 | 2.28 | <0.001** | 0.00 | - | - |
Tab. 5. Multivariate logistic regression analysis for independent predictors for recurrent uterine descent.
Discussion
The apical prolapse is probably the most complex form and the corner stone of pelvic organ prolapse (POP). Adequate apical support is essential in the treatment of POP, as it contributes to the support in all vaginal compartments. Anterior and posterior vaginal repairs may be unsuccessful if the apex is not well suspended. There are a variety of surgical treatments for vaginal apical prolapse, the ASC and the SSF are the most widely used procedures to repair apical prolapse [5].
In this study, we compared the early and late outcomes of two different surgical routes, the abdominal sacral hysteropexy and vaginal sacrospinous hysteropexy. The demographic data between the two groups was similar. We followed the patients for one year and found that recurrent cases were more frequent in SFF group than abdominal sacropexy group. There were 2 patients with recurrent uterine prolapse (5.4%) in the ASH group and 7 (20%) in the SSF group at 1 year post-operative, but to our point of view, the most important reasons for this might be that mesh is anchored to the anterior longitudinal sacral ligament or to the sacral bone (S2) during sacropexy, the stronger mesh may be responsible for the better success rate of sacral hystropexy compared to SSLF and the lower risk of both apical and total prolapse recurrence. It's also possible that massive vaginal dissection during SSF might cause neuropathy.
The number of patients needed another surgery as a total either for uterine or vaginal prolapses was statistically significant at one year post-operative. However, the re- operation rate for recurrent uterine prolapse only was insignificant between both groups, but higher in SSF group.
The overall risk for de novo cystocele and rectocele at one year was insignificant between the two groups, However, the risk of de novo cystocele was higher in SSF group (25.7%), as when the vaginal axis deviates too far to the back, the anterior vaginal wall loses its support. In contrary, the rate of De novo rectocele was higher in ASH group (10.8%) and this may be developed from the broader dissection of the posterior vaginal wall in the SSF group, so better correction of this area.
The operative time, blood loss and the duration of hospital stay were higher in ASH group. Blood transfusion, fever, wound infection, and visceral injuries were not significantly different between the two groups. Buttock pain was the most common complication of SSF, occurring in 2% of patients and possibly related to the levator ani nerve, which crosses the SSL at 0–4 cm medial to the ischial spine, or the pudendal nerve, which is inferior to the SSL and vaginal dissection that causes tension, but was self-limited. Only one patient experienced rectal injury. Wound complications occurred in 6 patients (16.6%) in ASH, higher than that reported in the literature and might be due to morbid obesity, concomitant vaginal surgery and presence of diabetes mellitus, the overall rate of complications were not different between the two groups.
One of the major complications that require reoperation in ASC is mesh erosion. Concomitant total hysterectomy increases the risk of mesh erosion after SCP up to seven- fold as reported by Rogers et al., [6]. We didn’t face such complication as we operated on preserved uterus.
According to Cochrane group, a systematic review of six randomized controlled trials done by Maher et al. [7]. Demonstrated that abdominal sacrocolpopexy was superior to vaginal sacrospinous fixation. SSF is associated with a higher risk of prolapse recurrence and repeat surgery for prolapse than SCP, with a shorter operating time and early daily activities being the only advantages. Awareness of prolapse was more common after vaginal procedures. Anterior and posterior compartment prolapses, Postoperative SUI were probably more common following the vaginal SSF. There was no evidence of a difference between the groups for bowel injury, the need for blood transfusion, length of hospital stay, de novo urge incontinence, sexual function and quality of life. The difference with our study merged from they demonstrate prolapse recurrence as a total including apical, anterior and posterior compartment prolapse unlike in our study we defined recurrence for apical prolapse and compared each compartment separately. They had a higher risk for vaginal prolapse and post-operative SUI in the SSF group and that may be due to the concomitant vaginal and anti- incontinence repair in our study.
In a meta-analysis performed by Zhang et al., [8], the operative time was significantly shorter in the SSF group. There was a significant difference between the SSF and sacrocolpopexy groups in terms of haemorrhage and wound infection. There was no difference in terms of tissue injury, cystocele and rectocele recurrence during the operation. The recurrence rate in SSF was significantly. Although it was higher in SSF group in our study, but not statistically significant. However, every study had its own definition of success and failure, thus it's impossible to compare the results across various studies because of the wide range of outcomes. There was also a high potential of bias due to the retrospective nature of the investigations, as well as inadequate random sequence generation and blinding.
In a prospective study done by Castro et al., [9], they reported that SSF presents a shorter operative time and duration for return to activities when compared with ASC with no statistically significant difference in the objective cure rate, but a significantly higher rate of rectocele in the abdominal group. This rate was not significant in our study, and this may be because they adopted excess vaginal dissection with concomitant posterior colporrhaphy in most cases of SSF group.
Our study differs with a retrospective study conducted by Isil Koleli and Ercan Yilmaz, [4], that showed, the subjective and objective success rate of ASC and SSF were similar on the 1st year after surgery which were higher in ASH group in our study. the cystocele rate in SSF was 8% lower than reported in literature 23%, while the rate of De novo cystocele in SSF group in our study was 25% similar to literature, but that because anterior colporrhaphy was performed at SSF operation concomitantly in their study.
Our results are similar to a retrospective study conducted by Sumin Oh et al., [10] comparing ASC and native tissue vaginal repair (NTVR), they reported that abdominal group was associated with a longer operating time and hospital stay, and more blood loss, but with higher surgical success rate, while the NTVR group had more cases of symptomatic and anatomic recurrence. Overall complication rates were similar. Also similar to a retrospective study done by Rogers et al., [6], that reported the same findings with points Ba and C were better in the ASC group, with PISQ-12 scores and quality of life showed no difference in improvement between groups. The difference with our study was that the total reoperation rate reported by Sumin Oh et al. [10] (including prolapse recurrence and complications) was significantly higher in the SCP group, unlike our study which was higher in SSF group, but the majority of reoperations were due to mesh erosion which didn’t occur in our study and and unlike the study of Rogers et al. [6] which was similar in both groups that may be due to a higher number of patients in their study who had undergone prior prolapse repairs which were excluded in our study, and a history of prior repair may have important implications on success of the current attempt at repair.
The points of strength in this study are first, its prospective nature that reduced error rates, selection bias, recall bias and unknown confounding variables, which may negatively affect the accuracy of the results, also this is one of the few studies that made such comparison on preserved uterus, second point was that both surgical routes were performed by the same team of expert urogynecologists in a tertiary center, university hospital so the discriminate level of surgeons that might affect the duration and outcomes of the procedures wasn’t found. Third point of strength, we used logistic regression models with adjustment for imbalanced baseline variables when outcome analysis was performed to minimize a possible confounding effect. Fourth point, we also had no patients drop out during the follow up period as we followed an accurate system for tracing the patients including scheduling visits and accessible communications. Fifth point, our study was also strengthened by the use of a validated measurable questionnaire to assess quality of life that had no concern in the previous studies.
The main limitation was the studies relatively short follow-up period, so it's possible that the risk of recurrence of POP, de novo SUI, or other side effects was underestimated in this investigation. The average mean follow-up period in literature is between 13.8 months and 4.8 years, according to published literature reviews. However, in our research, we had a 12-month follow-up. Another limitation was, patients with symptomatic pelvic prolapse seldom had a single compartment defect that raised the incidence of concurrent surgeries and hence increased the risk of adverse events, although this restriction was reported in practically all prior trials.
Conclusion
Abdominal sacral hysteropexy is associated with a lower risk of recurrence, but with significantly greater intraoperative blood loss and operative time, along with significantly more patients with postoperative pyrexia, Hospital stay and slower return to daily activities. The vaginal route may be preferable in women with medical disorders and obesity as it is associated with lower intra and postoperative morbidity with shorter operative time.
The Implication for Practice
The surgeon should consider presence of multiple risk factors for recurrence before choosing the surgical approach. Higher recurrence rates favor ASH, while minimizing adverse events and presence of medical co- morbidities favor SSF. Surgeons should also inform their patients about the potential downsides and upsides of certain surgical procedures, as well as provide information on other treatment choices. Because the incidence of de novo cyctocele was greater in the SSF group, the ASC operation should be used to treat apical prolapse in patients with anterior vaginal wall prolapse stage 2. Concomitant anterior colporrhaphy is preferable with SSF while concomitant repair of enterocele is preferable with ASH.
The Implication For Future Re-Search
More focus and action are needed to increase preventive, diagnostic, and treatment services for this serious health issue. We also need to develop longer-term clinical studies and compare with modern methods such as laparoscopic or robotic surgery and also in comparison with vaginal utero- sacral ligament suspension.
Authors Contribution
(A) Study Design· (B) Data Collection . (C) Statistical Analysis · (D) Data Interpretation · (E) Manuscript Preparation· (F) Literature Search · (G) Funds Collection
References
- Smith FJ, Holman CA, Moorin RE, et al. Lifetime risk of undergoing surgery for pelvic organ prolapse. Obstet Gynecol. 2010;116(5):1096-1100.
- Yoon I, Gupta N. Pelvic prolapse imaging. StatPearls Pub. 2019.
- Maher C, Feiner B, Baessler K, et al. Surgical management of pelvic organ prolapse in women. Cochrane Database Syst Rev. 2013(4).
- Köleli I, Yılmaz E. Vaginal sacrospinous ligament fixation versus abdominal sacrocolpopexy for the treatment of vaginal cuff prolapse: A retrospective study. 2019;26(3):398-403.
- Barber MD, Maher C. Apical prolapse. Int Urogynecol J. 2013;24(11):1815-33.
- Rogers RG, Nolen TL, Weidner AC, et al. Open sacrocolpopexy and vaginal apical repair: retrospective comparison of success and serious complications. Int Urogynecol J. 2018;29(8):1101-1110.
- Maher C, Feiner B, Baessler K, et al. Surgery for women with apical vaginal prolapse. Cochrane Database Syst Rev. 2016(10).
- Zhang W, Cheon WC, Zhang L, et al. Comparison of the effectiveness of sacrospinous ligament fixation and sacrocolpopexy: a meta-analysis. Int Urogynecol J. 2021;3:1-1.
- de Castro EB, Brito LG, Giraldo PC, et al. Does the vaginal flora modify when a synthetic mesh is used for genital prolapse repair in postmenopausal women? A Pilot, Randomized Controlled Study. Female Pelvic Med Reconstr Surg. 2019;25(4):284-288.
- Oh S, Shin EK, Hyun S, et al. Comparison of treatment outcomes for native tissue repair and sacrocolpopexy as apical suspension procedures at the time of hysterectomy for uterine prolapse. Sci Rep. 2021;11(1):1-7.
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Author Info
Ihab Gomaa, Mohammad NasrAl Deen, Tamer Farouk Borg, Mahmoud Ghaleb, Asmaa Ragab* and Basem Aly IslamCopyright:This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.