Case Report - (2022) Volume 17, Issue 4
A rare case reporting history of CS scar ectopic managed expectantly ending in placenta previa then its recurrence in next pregnancy and managed by hysteroscopic resection: A case report and literature review
Mohamed I Taema*, Ibrahim ali and Amr SobhyReceived: 14-Nov-2022, Manuscript No. gpmp-22-79689; Editor assigned: 16-Nov-2022, Pre QC No. P-79689; Reviewed: 29-Nov-2022, QC No. Q-79689; Revised: 07-Dec-2022, Manuscript No. R-79689; Published: 29-Dec-2022
Abstract
Introduction: A Cesarean scar ectopic pregnancy (CSEP) sometimes causes life-threatening bleeding and many treatment strategies have been proposed; expectant management, methotrexate administration, surgical evacuation, hysteroscopic resection, uterine artery embolization, or combination of them. We here report a patient: she had CSEP, which was managed expectantly and yielded placenta previa. Then, next, she had recurrent CESP, which was resected hysteroscopically with success.
Case Presentation: The patient had abdominal pain and vaginal bleeding. Ultrasound and magnetic resonance imaging revealed the image-findings indicative of CSEP compatible with 5 weeks of pregnancy. Hysteroscopic resection of CSEP was performed with success.
Conclusion: CSEP can recur and physicians should be aware of this. Hysteroscopic resection may be an option of the treatment of CSEP.
Keywords
Case report; Recurrent; CS scar ectopic; Placenta previa; Hysteroscopic resection
List of Abbreviations
CSEP: Cesaerean section ectopic pregnancy; CS: Cesaerean section; MRI: Magnetic Resonance Imaging; TVS: Transvaginal sonography; G: Gravida; P: Para
Introduction
A cesarean scar ectopic pregnancy (CSEP) is an implantation of pregnancy in the myometrium of lower uterine segment of a previous cesarean section scar. It is a rare condition and occurs in approximately one in every 2000 patients who have had a previous cesarean section [1]. Its incidence has increased with the increase in number cesarean deliveries. It carries a greater risk of maternal hemorrhage and ultimately maternal mortality. There are many modalities of options for treatment including expectant management, methotrexate, surgical evacuation or hysteroscopic resection, intervention radiological uterine artery embolization or a combined approach[2]. The level of success of each modality is dependent on the surgeonâ??s skill and patient condition and choice. To the best of our knowledge that this is the first case to have a CSEP to be managed expectantly (and became a placenta previa in last pregnancy) and to recur in next pregnancy as CSEP.
Case Presentation
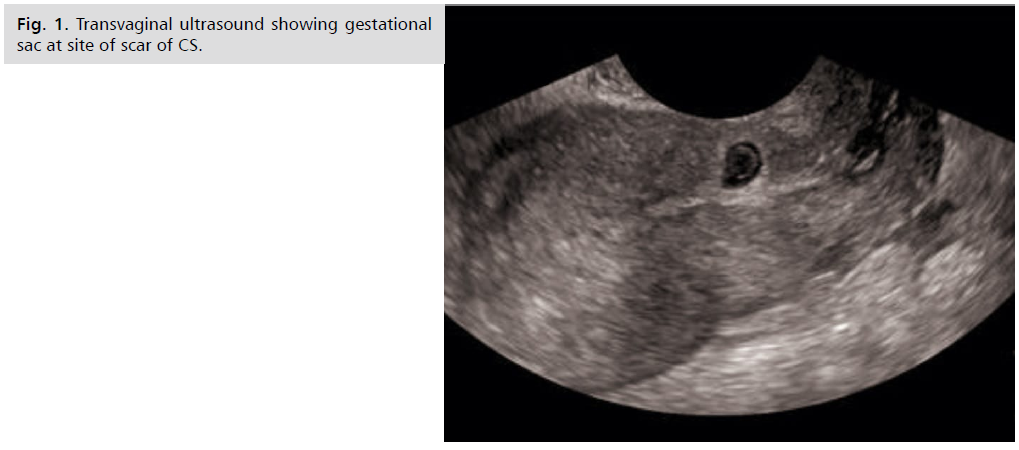
Patient specific information is not mentioned. She is G9P5+3 all deliveries by CS. The Primary concern of the patent is to prevent the occurrence of placenta accreta spectrum and its consequence of blood transfusion and peripartum hysterectomy. Obstetric history includes 5 previous CS with last one was LSCS with midline laparotomy incision for placenta previa. Just before pregnancy was CSEP and end up in placenta previa. Physical examination (PE) revealed normal vital data, tenderness and rigidity all over the abdomen and marked cervical motion tenderness. Diagnostic testing done was BHCG was 7661miu/ml then repeated after 48 hours to be 18533 MIU/ML (Fig. 1.). TVS revealed an intrauterine gestation seen in the lower uterine segment near the location of the C-section scar. There was significant thinning of the myometrium, and the gestational sac showed a smooth shape. A double wall sign was observed, and a yolk sac was identified within the gestational sac. However, no fetal pole was visible. The gestational sac measured 1.49 cm GA =5W 3D (picture suggestive of C.S scar ectopic pregnancy), correspondingly MRI of the pelvis was performed and showed the presence of a gestational sac measuring 3.2 x 1.5 x 2.1 cm within the endometrial cavity. The sac was protruding through the myometrium in the lower uterine segment, namely in the area of the Cesarean section scar. There were no diagnostic problems for this instance. The diagnosis was confirmed as recurrent CSEP.
Fig 1. Transvaginal ultrasound showing gestational sac at site of scar of CS.
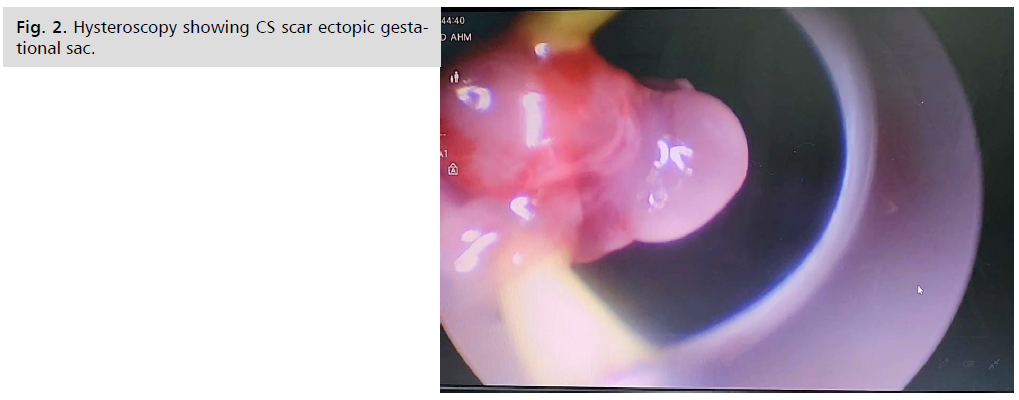
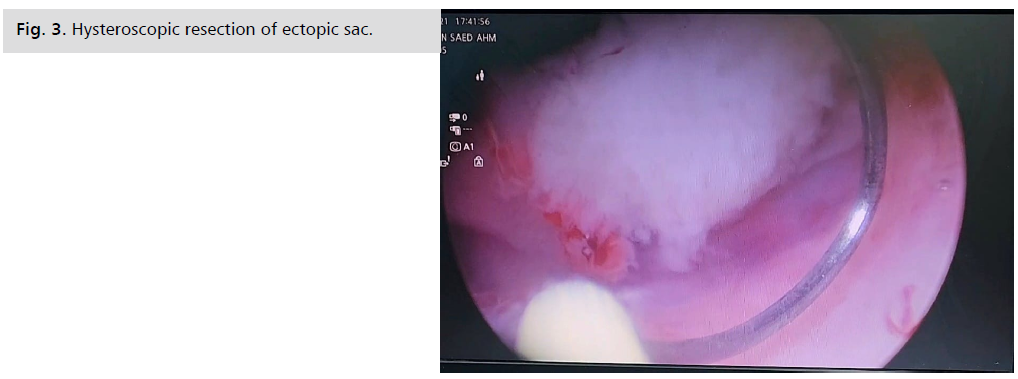
Hysteroscopic intervention was decided and the procedure began with cervical dilatation till Hegar dilator no 8, resectoscope was introduced revealing scar ectopic pregnancy with its lower pole attached to cesarean section scar(Fig. 2.), resection of the lower pole was done (Fig. 3.) then suction curettage then insertion of intrauterine balloon tamponade (foleyâ??s catheter) filled with 50 ml saline. The procedure took around 60 minutes .The patient tolerated the procedure well with no Adverse and unanticipated events.
Fig 2. Hysteroscopy showing CS scar ectopic gestational sac.
Fig 3. Hysteroscopic resection of ectopic sac.
2nd day post-operative B-HCG was 3760, the intrauterine bleeding was minimal and the intrauterine catheter was removed after 48 hours. The patient was discharged after 72 hours.
Discussion and Literature Review
The initial occurrence of a clinically significant case of CSEP was documented in the medical domain in 1978, involving a 23-year-old female from South Africa [3].
Due to the rising frequency of caesarean sections in recent decades, there has been an increase in the occurrence of prenatal anomalies, leading to a greater focus on these conditions by physicians. The literature reports that the incidence of CSEP ranges from 1 in 1800 to 1 in 2216 pregnancies, with a prevalence of 0.15% in cases with previous caesarean procedures. Furthermore, the risk of CSEP is increasing with the frequency of repeated cesarean sections [4].
The etiology of this condition remains uncertain. A variety of theories have been proposed to explain this phenomenon: (a) the gestational sac moves internally either through a small opening within the cesarean section scar or a defect in the lower uterine segment; (b) the placental villi invade the uterine wall at the site of scar dehiscence, and (c) the fertilized egg implants in areas of scar tissue with low oxygen levels [5].
This text explains the pathology that occurs in cases where previous procedures such as cesarean section (CS), myomectomy, dilatation and curettage (D&C), hysterotomy, manual removal of placenta, and/or abnormal placentation in vitro fertilization (CSEP) are present. The pathology can be attributed to defects in the scar tissue formed during the previous procedures, which can lead to the development of a microtubular tract due to poor healing of the trauma caused by these procedures [6].
The pathophysiology of scar pregnancy differs from that of an intrauterine pregnancy with placenta accreta. In situations of placenta accreta formation, the products of conception are mainly found in the uterine cavity. The main cause of the invasion of the myometrium by trophoblastic tissues to variable degrees is the absence of decidua basalis [7]. In cases of scar pregnancy, the myometrium and fibrotic tissues of the scar fully enclose the gestational sac, effectively separating it from the endometrial cavity [7].
The weak vascular support in the anterior uterine wall, specifically in patients with a history of previous caesarean section procedure, is the primary factor responsible for this pathology. In these cases, blastocyst implantation occurs in the area of fibrous scar tissue created by the previous caesarean section, before the formation of decidua basalis, and extends to the myometrium [8].
There are two types of scar pregnancy. Type I endogenic form is the result of the gestational sac being implanted in the scar tissue from a previous caesarean surgery, with expansion towards either the cervico-isthmic space or the uterine cavity [6,7]. .In this scenario, a profound infiltration into a cesarean scar tissue defect towards the urinary bladder and the abdominal cavity is accompanied by numerous unfavorable pregnancy outcomes, including a ruptured uterus, uncontrollable bleeding, the need for emergency laparotomy and hysterectomy, and even maternal mortality. Type II, also known as exogenic form, refers to the growth of implantations inside the uterine cavity [6]. Type II is the result of the implantation of tissues into scar defects, with infiltration and expansion into the uterine myometrium and serosal surface. This can cause a ruptured uterus and severe hemorrhage during the first trimester of pregnancy. There is a risk of fertility loss if massive hemorrhage occurs, and emergency laparotomy and hysterectomy are required [7].
The symptoms of this condition include vaginal bleeding and stomach pain during the first trimester of pregnancy. However, it is important to note that many women may not experience any symptoms when diagnosed [9].
Transvaginal ultrasonography is considered the most reliable method for diagnosing CSEP in the first or early second trimester. This method provides high-resolution images. It is recommended to combine color Doppler with grayscale evaluation to enhance visualization of the placental site implantation and to define extraembryonic and fetal structures in more detail [10]. The Type I "on-thescar" or endogenic form is characterized by a significant ultrasonographic clear layer of myometrium between the anterior wall of the uterus and the developed placenta. The ultrasonographic images of Type II "in-the-niche" or exogenic form reveal a narrow myometrial interface beneath the placenta.
The ultrasound findings suggestive of CSEP may include: (1) an empty endocervical and endometrial cavity; (2) a nested gestational sac and placenta in the area of the previous scar; (3) the scar "niche" filled by a triangular, rounded, or oval-shaped gestational sac; (4) a thin or absent myometrial layer between the bladder and the gestational sac; (5) a unique or highly vascular pattern around the scar area; and (6) the presence of an embryonic or fetal pole, yolk sac, or both, with or without fetal cardiac activity. The presence of a protrusion or swelling in the middle line of the bottom part of the uterus, as seen in a transabdominal view, indicates the diagnosis of CSEP [10,11]
To ensure optimal results from initial diagnosis and treatment, it is recommended that pregnant women with a history of previous caesarean sections undergo a first trimester scan at the Early Pregnancy Assessment Clinic following a positive pregnancy test. Transvaginal ultrasonography (TVS) is still the preferred method of assessment. In some situations, an abdominal ultrasound may be used in addition to provide a wider picture, and threedimensional Power Doppler can be used to validate ultrasound findings. Magnetic resonance imaging (MRI) can be used to confirm the initial diagnosis made through ultrasonography in circumstances when there is uncertainty [12].
The treatment options include expectant management (which has recently been partially withdrawn based on recommendations from the Society for Maternal-Fetal Medicine), medical management with methotrexate, and surgical intervention. The mode of treatment is determined primarily by the case presentation and clinical symptoms [10]. The existing literature strongly supports surgical management over medicinal modalities based on the success rates. However, it is important to note that the data primarily come from case series, as stated in the latest recommendations by the Society for Maternal- Fetal Medicine [10,13]. Given the nature of CSEP, it is anticipated that there may be clinical symptoms and associated consequences, which may be more severe in their expression. Thus, surgical intervention continues to be the most effective and well accepted treatment procedure, often used in combination with other available approaches. In addition to hysteroscopic treatment, other surgical methods as laparoscopic or laparotomic excision, vacuum aspiration, and suction can also be utilized to remove scar pregnancy [10]. The current treatment options for CSEP (Cesarean scar ectopic pregnancy) include medicinal management, followed by uterine surgical treatment, typically using minimally invasive techniques such as laparoscopic uterine incision and removal of the scar pregnancy foci. Other options include complete laparoscopic hysterectomy (TLH) and vaginal incision of the uterus with removal of the CSEP pregnancy then restoration of the uterine muscular wall, as well as selective uterine artery embolization (UAE) [14].
Management of CSEP in the first and early second trimesters should be conducted in a well-equipped facility that offers a range of therapeutic options and blood bank services. All hemodynamically unstable patients should undergo immediate surgical intervention, preferably using a minimally invasive method. Management options for individuals who are stable in terms of their hemodynamics include either surgical or medical termination of pregnancy, or in certain exceptional circumstances, continuation of the pregnancy. For persons with a fetal demise in cases of CSEPs, a possible approach could be to consider expectant management along with medical or surgical treatment [11,15]. Patients with Type I rather than Type II CSEPs tend to have more favorable results with expectant treatment, particularly when the myometrial thickness is ≥ 3 mm [16].
The CSEP can be surgically removed via hysteroscopy, laparoscopy, or laparotomy [17]. Suction aspiration with guided ultrasound is an alternative to the conventional CSEP method for terminating pregnancies in the early first trimester (5 to 7 weeks). In cases when there is significant bleeding, a transcervical balloon catheter is used in addition to the procedure. Transvaginal or transabdominal intra-gestational injection of methotrexate (MTX) under ultrasonographic guidance is an alternative treatment option for CSEP in the early first trimester (6 to 8 weeks), with a success rate of 85%. However, its effectiveness becomes more challenging to predict in more advanced pregnancies [17]. Administration of a potassium chloride (KCl) solution via injection. Transabdominally or transvaginally, under ultrasonographic guidance in a CSEP with fetal cardiac activity has also been documented, with the injection of 5 mEq into the gestational sac [18]. Systemic MTX can be used as an additional treatment alongside all of the mentioned methods [19].
Once the diagnosis of CSEP is confirmed, prompt treatment should be initiated without any delay. A rapid choice for termination should be made due to the heightened risk of bleeding if the pregnancy is allowed to continue [4]. The primary objective of the procedure is to end the pregnancy by removing the gestational sac while ensuring the patient's ability to conceive in the future. Presently, the majority of research supports the recommendation that patients with severe type I or type II CSEP should undergo UAE (uterine artery embolization) treatment. This procedure is linked to a significant reduction in the risk of intraoperative bleeding [14].
There have been only a few recorded cases of laparoscopic management of CSEP. Kathopoulis et al. have published their experience with laparoscopic treatment in two instances, employing various operational approaches. Laparoscopic care of CSEP is considered necessary when the ectopic pregnancy is developing towards the urinary bladder and abdominal cavity (type II CSEP), either as a primary intervention or after medicinal treatment has failed [20]. A laparoscopic procedure to remove CSEP during the first eleven weeks of pregnancy has also been documented [21]. The primary benefit of the laparoscopic method is the thorough extraction of the retained products of conception during the surgery, resulting in a reduced need for further follow-up appointment [4]. Furthermore, the restoration of the uterine anatomy in the lower segment enhances the likelihood of positive reproductive outcomes in the future [22].While being a dependable management strategy, it should be performed by proficient laparoscopic surgeons
The strength of this case report is that it is the first in which a CSEP was managed optimistically (and became a placenta previa in the previous pregnancy) and recurred as a CSEP in the next pregnancy. The drawback is that we do not have the investigations and MRIs from earlier CSEPs that resulted in placenta previa.
The message from this case report is that we are hesitant to reassure surgeons about the expected management of CSEP, even if it is of the endogenous type, because the danger of placenta accreta or recurrence in the following pregnancy remains significant.
Conclusion
CSEP is a rare obstetrical illness that can put a woman's life in danger, such as a ruptured uterus or extensive hemorrhage, which can lead to maternal death. This circumstance provides a significant diagnostic problem in our obstetrics and gynecology clinical sector, and timely and meticulous decisions should be made as soon as possible. Clinicians should use transvaginal ultrasonography as their primary diagnostic technique. Women should have full access to all acceptable CSP treatment alternatives.
Management is frequently individualized, as in our instance, where the decision for hysteroscopic resection treatment options was taken in the concept of personalized medicine and the best management of such a lifethreatening condition.
Patient Perspective
Patient was satisfied with the procedure done as she is convinced that expectant management done in previous CSEP would have endangered her life. The patient gave informed consent and it’s available upon request.
Declaration
Ethics approval and consent to participate: An informed consent was taken from the patient to publish the case, No IRB is needed from our hospital in surgical case reports.
Consent for Publication
The patient gave the consent to publish case.
Availability of Data and Materials
Available upon request.
Competing Interest
Authors declare no conflict of interest.
Funding
No funding for this case report.
Authors Contribution
(A) Study Design · (B) Data Collection · (C) Statistical Analysis · (D) Data Interpretation · (E) Manuscript Preparation · (F) Literature Search · (G) No Fund Collection
References
- Morente LS, León AI, Reina MP, et al. Cesarean Scar Ectopic Pregnancy—Case Series: Treatment Decision Algorithm and Success with Medical Treatment. Medicina. 2021;57(4):362.
- American College of Obstetricians and Gynecologists. Tubal ectopic pregnancy. ACOG Practice Bulletin No. 193. Obstet Gynecol. 2018;131(3):e91-103.
- Marchiole P, Gorlero F, De Caro G, et al. Intramural pregnancy embedded in a previous Cesarean section scar treated conservatively. Ultrasound Obstet Gynecol. 2004;23(3):307-309.
- Gonzalez N, Tulandi T. Cesarean scar pregnancy: a systematic review. J Minim Invasive Gynecol. 2017;24(5):731-738.
- Jauniaux E, Collins S, Burton GJ. Placenta accreta spectrum: pathophysiology and evidence-based anatomy for prenatal ultrasound imaging. Am J Obstet Gynecol. 2018;218(1):75-87.
- Majangara R, Madziyire MG, Verenga C, et al. Cesarean section scar ectopic pregnancy-a management conundrum: a case report. J Med Case Rep. 2019;13(1):1-4.
- Patel MA. Scar ectopic pregnancy. J Obstet Gynaecol India. 2015;65(6):372-375.
- Aslan M, Yavuzkir Ş. Suction Curettage and Foley Balloon as a First-Line Treatment Option for Caesarean Scar Pregnancy and Reproductive Outcomes. Int J Womens Health. 2021;13:239.
- Agten AK, Cali G, Monteagudo A, et al. The clinical outcome of cesarean scar pregnancies implanted “on the scar” versus “in the niche”. Am J Obstet Gynecol. 2017;216(5):510-510e1.
- Miller R, Timor-Tritsch IE, Gyamfi-Bannerman C, et al. Society for Maternal-Fetal Medicine (SMFM) consult series# 49: cesarean scar pregnancy. Am J Obstet Gynecol. 2020;222(5):B2-14.
- Timor-Tritsch IE, Khatib N, Monteagudo A, et al. Cesarean scar pregnancies: experience of 60 cases. J Ultrasound Med. 2015;34(4):601-610.
- Panaiotova J, Tokunaka M, Krajewska K, et al. Screening for morbidly adherent placenta in early pregnancy. Ultrasound Obs Gynecol. 2019;53(1):101-106.
- Petersen KB, Hoffmann E, Larsen CR, et al. Cesarean scar pregnancy: a systematic review of treatment studies. Fertil Steril. 2016;105(4):958-967.
- Guo J, Yu J, Zhang Q, et al. Clinical efficacy and safety of uterine artery embolization (UAE) versus laparoscopic cesarean scar pregnancy debridement surgery (LCSPDS) in treatment of cesarean scar pregnancy. Med Sci Monit. 2018;24:4659.
- Calì G, Timor‐Tritsch IE, Palacios‐Jaraquemada J, et al. Outcome of Cesarean scar pregnancy managed expectantly: systematic review and meta‐analysis. Ultrasound Obstet. 2018;51(2):169-175.
- Karakuş R, Karakuş SS, Güler B, et al. Myometrial thickness overlying cesarean scar pregnancy is significantly associated with isthmocele formation in the third month of the postoperative period. Turk J Obstet Gynecol. 2021;18(1):37.
- Zhang X, Pang Y, Ma Y, et al. A comparison between laparoscopy and hysteroscopy approach in treatment of cesarean scar pregnancy. Medicine. 2020;99(43).
- Nippita S, Carranza AS, Paul ME. Funic potassium chloride injection during intact dilation and evacuation. Contraception. 2021;104(3):275-277.
- Collins SL, Alemdar B, van Beekhuizen HJ, et al. Evidence-based guidelines for the management of abnormally invasive placenta: recommendations from the International Society for Abnormally Invasive Placenta. Am J Obstet Gynecol. 2019;220(6):511-526.
- Kathopoulis N, Chatzipapas I, Samartzis K, et al. Laparoscopic management of cesarean scar pregnancy: Report of two cases with video-presentation of different operative techniques and literature review. J Gynecol Obstet Hum Reprod. 2021;50(8):102066.
- Pickett CM, Minalt N, Higgins OM, et al. A laparoscopic approach to cesarean scar ectopic pregnancy. Am J Obstet Gynecol. 2022;226(3):417-419.
- Wu J, Ye J, OuYang Z, et al. Outcomes of reproduction following cesarean scar pregnancy treatment: A systematic review and meta-analysis. Eur J Obstet Gynecol Reprod Biol. 2021;262:80-92.
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Author Info
Mohamed I Taema*, Ibrahim ali and Amr SobhyCopyright:This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.